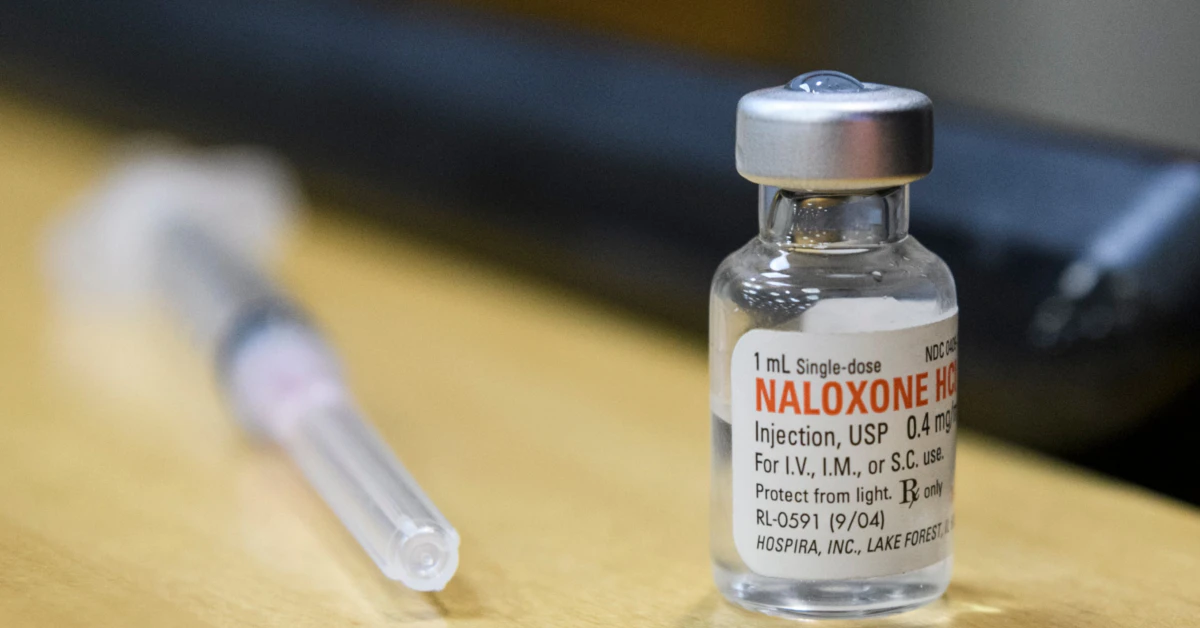
Let’s get right to it: Yeah, most Medicaid plans cover naloxone—the drug that reverses opioid overdoses. But here’s the kicker: coverage doesn’t always mean you can walk into a pharmacy and grab it. Restrictions, paperwork, and quantity limits still trip people up. Worse? Three states keep it completely off their Medicaid radar. If you’re relying on these plans for protection, we’re diving into exactly how to navigate these roadblocks.
Real talk: If an opioid overdose happens, you don’t have time to argue with red tape. You need naloxone now. That’s why this isn’t just about what’s technically available—it’s about whether people who need it can bypass the hoops and get help fast. Let’s unpack the facts, the frustrations, and the fight for straightforward access.
You’ve Got Coverage—But Wait, What’s the Catch?
Okay, imagine this: You’re told you’re “covered” for something critical. Then… you call a pharmacy and hear, “We’ll need pre-approval, and we can only dispense two doses… per year.” Frustrating? Absolutely. A recent study shows nearly all Medicaid plans technically cover naloxone. But the devil is in the details. Even though the drug’s there on paper, access isn’t a walk in the park for tens of millions of people.
Let’s break it down like we’re talking over coffee:
What Do Restrictions Really Look Like?
Maybe you’ve heard Medicaid covers naloxone and thought, “Great, less to sweat over.” But what if I told you that “coverage” isn’t a green light? Some plans slap quantity limits—like only two doses a year. Others make you jump through prior authorization hoops, which is a fast way to waste precious minutes.
Here’s the lowdown:
State-by-State Naloxone Restrictions
| State | Quantity Limits | Prior Authorization Required? | Total Medicaid Coverage for Naloxone |
|---|---|---|---|
| Florida | 2 doses/year | No | ✅ |
| Texas | 1 dose/year | Yes | ✅ |
| Ohio | N/A | N/A | ❌ |
| Kentucky | N/A | N/A | ❌ |
| Tennessee | N/A | N/A | ❌ |
You’re probably wondering, “Wait, how does ‘coverage’ work if there are rules that make it hard to use?” Great question. Let’s dig deeper.
Overdose Survivors Need This Drug Before It’s Too Late
D’you know what’s wild? The people on Medicaid have twice the overdose risk of the general population, according to Medicaid Managed Care Naloxone Coverage and Management research. Yet the system isn’t doing nearly enough to make sure naloxone is where it needs to be. It’s like giving someone a life jacket—but then not letting them wear it during a storm.
Why Is Easy Naloxone Access a Life-or-Death Issue?
Imagine this: Your cousin, who uses street drugs, is at your birthday party. Suddenly, their breathing changes—slower… then stops. Would you pause to call Medicaid for paperwork? Nope. Survival depends on having naloxone in your hand, not buried in a maze.
Different formats exist—nasal spray is the easiest to use, injectables for professionals, auto-injectors for quicker delivery. But some plans only cover one of these. Why? “Cost reasons.” It’s a little messed up, especially when delaying action means losing someone.
What’s the Real Cost of Quantity Limits?
Here’s a scenario that plays out far too often: A guy in Ohio helps a friend after an overdose. He uses his single naloxone dose to save a life. Fast-forward: Someone else overdoses at his house. No naloxone to spare because Medicaid says “wait six months for a refill.”
Quantity limits aren’t just numbers—they’re barriers at the worst possible moments. And if you live in a high-risk area, that number you see on the plan’s website feels hollow.
Home States? Some Slap the Shutters Closed
If you’re in Kentucky, Ohio, or Tennessee and rely on Medicaid, you’re completely outta luck. Reports say those states don’t cover naloxone through their Medicaid managed care at all. Unbelievable, right? With overdose rates spiking, this feels like leaving a lifeline up to chance—and local advocates are saying loud and clear, “This isn’t okay.”
Why Are These States Falling Behind?
Some of these regions are in the middle of acute opioid crises. So it’s a real messy situation when Medicaid won’t back the best-known overdose reversal tool. Lack of political support? Budget issues? Misguided stigmatization of people who use drugs?—you’ll have to talk to local policy folks.
Here’s the thing, though: You don’t fix a public health emergency by pretending the tools don’t exist. And when anyone—regardless of income—can’t get naloxone in the most dangerous parts of the country, we’ve got a giant problem.
How to Soften the Sting of These Medicaid Blocks
I won’t sugarcoat it—it’s rough. But there are ways we can push back. And if you’re in a better-covered state, your awareness can fuel change elsewhere.
Steps to Take If Your Medicaid Plan Sidelines Naloxone
Here’s your toolkit:
- Request an exception: Got a doctor who thinks you should have extra? They can file an appeal.
- Know your local rules: Medicaid policies vary by state. Sometimes different counties have different quirks.
- Seek local harm reduction groups: Many give out naloxone kits free with overdose prevention training.
And if it’s easier to go this route—y’know, great. But it shouldn’t have to be that hard.
For Policymakers—Because It’s Time to Step Up
We’ve seen states like Massachusetts push for full formulation coverage, dump quantity restrictions, and say, “Prior authorization? Not anymore.” This isn’t rocket science. These moves lift overdose reversals, reduce ER visits, and normalize naloxone as basic public health stuff, not a ‘luxury.’
If Medicaid is supposed to protect people, isn’t this like—style 101 for the program? Your thoughts? Or have I gone too hard on understaffed state bureaucracies? (I mean, they’re busy. But still.)
So What’s the Point of This Whole Thing?
Naloxone access is a cornerstone of survival in the opioid crisis. Medicaid covers it in most places—a win, for sure. Yet all these restrictions make you wonder: “Is it really accessible, or are we just pretending it’s enough?”
Yes, Restrictions Are Meant to Curb Fraud—and Bah Humbug to That
The folks arguing for laying down rules say it’s about “preserving resources” and “preventing diversion.” But in reality, these rules leave people high and dry when situations are dire. Only covering nasal spray? That’s fair if other formulations aren’t medically necessary. But no dose when you need it? That’s a bridge too far, medically speaking.
Do You Trust Your Medicaid Plan?
You probably sense this, but trust is within Medicaid threads like cracks in the sidewalk. Scenarios where you run out, can’t afford the deductible, or face forms that take days to clear just erode confidence over time. And when you don’t trust a system, you push harder for reform. That’s not just practical—it’s sane.
Why the Big Fat “Covered” Label Isn’t the End of the Story
Again, coverage ≠ access. Citing NIH findings, rules for medications like naloxone play with the lives of millions on Medicaid. So, yes, it’s been rolled out in local systems. But if it’s boxed in by quantity limits, capped at just nasal spray, or totally absent in three states, what’s the goal?
This is more than a Medicaid debate. This is about making sure opioids don’t cut someone’s life short when a $150 shot could avert disaster. And while price tags matter, so does the speed of action.
Wrapping It Up: Naloxone’s Worth a Fight
So here’s the truth:
- Over 70 million Medicaid folks in 40 states have naloxone coverage. That’s a win.
- But red tape still blocks access—quantity limits, prior authorization, or no coverage at all in some places.
- If you’re affected, you’ve got options: talk to providers, fight denials, or lean on local harm reduction resources.
It’s okay to be angry. Empathy is okay. And action is necessary. Your next step? Share this post with others who might need—ahem—real info. Or call your state Medicaid office. Because this isn’t just about naloxone access. It’s about fairness, science, and putting people before policy fatigue.
Ask yourself this: What’s the point of a life-saving tool if it takes a week just to get it approved? You don’t get extended lifelines in overdose situations. We need to act like it.






















Leave a Reply
You must be logged in to post a comment.