Need to know right now if you’ve caught COVID‑19? The quickest way is to match the test to your symptoms, exposure risk, and how fast you need answers. No more scrolling through endless pages—this guide will walk you through every option, explain what the results really mean, and show you how to act with confidence.
From rapid antigen strips you can pop in your pocket to lab‑based PCR tests that hunt every viral whisper, we’ll break down the pros, the cons, and the perfect moments to use each one. Grab a coffee, stay comfortable, and let’s get you the clear, trustworthy info you deserve.
Why Test Matters
Testing isn’t just a checkbox; it’s a primary line of infection prevention. When you know your status, you can:
- Isolate before you spread the virus to family, coworkers, or strangers.
- Access treatments that work best when started early.
- Travel, attend events, or return to work with peace of mind.
- Help public‑health officials track outbreaks and allocate resources.
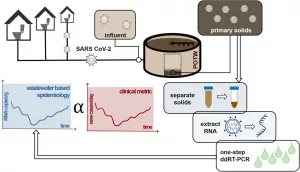
Think of testing as the “early warning system” for a respiratory virus screening program—it saves lives by catching infections before they cascade.
Test Types Overview
The world of COVID‑19 testing can feel like a candy store with too many flavors. Below is a quick snapshot of the three main families you’ll encounter.
| Test Type | How It Works | Time to Result | Accuracy |
|---|---|---|---|
| NAAT (PCR) | Amplifies viral RNA in a lab | 24‑72 hrs (some point‑of‑care < 30 min) | Very high – gold standard |
| Antigen | Detects viral proteins (spike) | 15‑30 min (on‑site or at‑home) | Good for symptomatic, lower for asymptomatic |
| Antibody (Serology) | Measures immune response | Hours‑days (lab) | Shows past infection, not current |
According to CDC guidance, NAATs (including PCR) remain the most reliable for diagnosing an active infection, while antigen tests shine when you need speed.
Pick the Right Test
Symptomatic vs. Asymptomatic
If you’re already feeling feverish, sore throat, or a sudden loss of taste, a PCR or a high‑quality antigen test will give you the clearest answer. For people who feel fine but suspect exposure, start with a rapid antigen test on day 5 after contact; if it’s negative but you still feel uneasy, follow up with a PCR.
High‑Risk Settings
Schools, nursing homes, and densely packed workplaces demand a careful testing cadence. Weekly antigen screening paired with confirmatory NAAT for any positive result keeps outbreaks in check while minimizing disruption. Learn more about protecting high-risk settings.
Cost and Access
Many states still offer no‑cost testing sites—just search your local health department or the CDC testing locator. Over‑the‑counter antigen kits are now on pharmacy shelves, but remember: a positive self‑test is reliable; a negative one may need a second check, especially if you have symptoms.
Special Populations
Pregnant folks, immunocompromised patients, and young children often benefit from the higher sensitivity of NAATs. A pediatric infectious‑disease specialist will typically recommend a lab‑based PCR to avoid missed cases.
How to Collect Sample
Nasal Swab vs. Saliva vs. Throat
A nasal swab—those short, fluffy sticks you see in clinics—is the most common specimen for both PCR and antigen tests. Saliva tests are gaining traction because they’re less invasive, but they’re not yet as widely available. Throat swabs can work for certain PCR kits but feel a bit more uncomfortable.
Here’s a quick, friend‑to‑friend guide for a nasal swab:
- Wash your hands thoroughly.
- Tilt your head back slightly.
- Insert the swab about ½ inch into one nostril, gently rotating for 5 seconds.
- Repeat in the other nostril with the same swab.
- Place the swab in the transport tube or testing device as instructed.
Need a deeper dive on the swab process? Check out our article on nasal swab test for step‑by‑step photos.
Preparing for Your Test
- Don’t eat, drink, smoke, or chew gum 30 minutes before a PCR swab.
- Avoid nasal sprays or decongestants for a few hours.
- Bring a photo ID and any insurance information.
- Write down the exact time you were exposed—this helps clinicians pick the right testing window.
What Happens After the Sample?
For NAATs, the swab travels to a certified lab where technicians amplify any viral RNA. Results usually appear in your patient portal within 24‑72 hours. Antigen tests, on the other hand, give you a visual line or a digital readout right there on the spot.
Read Your Results
Positive Result
A positive test tells you the virus is present. Immediately:
- Isolate in a separate room, use a dedicated bathroom if possible.
- Notify anyone you’ve been in close contact with in the past 48 hours.
- Consider antiviral treatment (e.g., Paxlovid) if you’re eligible—early therapy can cut the risk of severe illness.
- Follow CDC’s isolation guidance: at least 5 days from symptom onset, plus 24 hours fever‑free without medication, and improving symptoms.
Negative Result
A negative result means the test didn’t detect the virus. But “negative” isn’t always final:
- If you tested before day 5 after exposure, the virus might still be below detection levels—retest on day 5 or later.
- If you have symptoms, a single negative antigen test should be confirmed with a PCR.
- Think of a negative as “no virus detected right now,” not a lifelong clearance.
False‑Positives and False‑Negatives
Every test has a tiny chance of error. False‑positives are rare with PCR but can happen with antigen kits if the device is contaminated. False‑negatives are more common with rapid tests, especially in asymptomatic people. That’s why the CDC recommends repeating a negative antigen test up to three times, spaced 48 hours apart, for greater confidence.
Practical Tips for Everyday Life
- Keep a small test kit in your bag—just in case you need a quick check before a meeting.
- If you’re traveling, verify the destination’s testing requirements—some airlines still ask for a recent PCR.
- Use a symptom‑tracker app to log when you first felt ill; it helps you pinpoint the optimal testing window.
- Stay current on respiratory virus screening guidance, especially during flu season when co‑infections are possible.
- When in doubt, ask your healthcare provider—better to double‑check than to wonder “what if?”
Takeaway
Choosing the right COVID‑19 test isn’t a one‑size‑fits‑all decision. Match the test to your symptom status, exposure risk, and how quickly you need answers. NAAT (PCR) gives you the highest accuracy, especially for high‑risk or symptomatic situations. Antigen tests are fast, affordable, and great for routine screening, but a negative result may need confirmation. Keep an eye on the timing of your test—testing too early can miss the virus, while testing too late can delay needed care.
By staying informed and using the appropriate test at the right moment, you protect not only yourself but also the people you love and the communities you belong to. If you’ve just gotten a result, share your experience with us or explore more about virus detection to stay ahead of the curve.






















Leave a Reply
You must be logged in to post a comment.