Most people don’t realize that everyday actions—hand hygiene, proper screening, and a few simple workflow tweaks—can dramatically curb the spread of viral respiratory infections in hospitals, clinics, and long‑term‑care homes. Below you’ll find the most actionable infection prevention strategies you can start using today, backed by CDC guidance and real‑world case studies. Let’s dive in together.
Why It Matters
Imagine walking into a bustling ward and feeling confident that every patient, visitor, and staff member is protected. That confidence isn’t a fantasy; it’s the result of solid infection prevention practices. Health‑associated infections (HAIs) affect roughly 1 in 31 hospitalized patients in the United States, according to the CDC’s infection‑control data. Those numbers translate into thousands of extra days in the hospital, added medical expenses, and, most heartbreakingly, preventable suffering.
Beyond the numbers, infection prevention safeguards the people we care about—the patients who rely on us for healing, the colleagues who share the same break room, and even our own families when we head home after a shift. When we get it right, we protect lives, preserve resources, and build a culture of safety that reverberates throughout the entire health system.
Core Pillars
Infection prevention rests on three foundational pillars: Standard Precautions, Transmission‑Based Precautions, and Targeted Screening. Think of these as the three legs of a sturdy stool—remove one, and the whole thing wobbles.
| Pillar | Key Actions | Quick Example |
|---|---|---|
| Standard Precautions | Hand hygiene, PPE use, safe injection practices | Perform the “5 Moments for Hand Hygiene” before every patient contact |
| Transmission‑Based Precautions | Identify droplet, airborne, or contact spread; isolate accordingly | Place a patient with confirmed influenza in a droplet‑precaution room |
| Targeted Screening | Respiratory virus screening, COVID‑19 testing, nasal swab testing | Use a rapid nasal swab test on admission during flu season |
Standard Precautions – The Universal Baseline
These are the “common sense” practices that apply to every patient, every time. Hand hygiene remains the single most effective measure. The CDC recommends washing hands for at least 20 seconds with soap and water, or using an alcohol‑based hand rub if hands aren’t visibly soiled. Think of it as the digital “refresh” button for your immune defenses.
PPE (personal protective equipment) isn’t just for high‑risk procedures. Gloves, gowns, eye protection, and masks should be selected based on the anticipated exposure. A quick rule of thumb: if there’s any chance of splashes or droplets, cover up. And remember, the right PPE won’t protect you if you skip the hand hygiene step before and after donning it.
Transmission‑Based Precautions – Targeted Defense
When you know a patient is carrying a specific pathogen, you add another layer of protection. The three categories are:
- Droplet Precautions: For organisms spread by large respiratory droplets (e.g., influenza, COVID‑19). Use surgical masks and maintain a 3‑foot distance.
- Airborne Precautions: For tiny particles that stay aloft (e.g., measles, varicella). Require N95 respirators and negative‑pressure rooms.
- Contact Precautions: For pathogens that survive on surfaces (e.g., MRSA, C. difficile). Gloves and gowns are a must, and clean room surfaces frequently.
Applying the correct category can feel like a puzzle, but a simple flowchart on the unit wall can guide staff in seconds. The payoff? Fewer secondary infections and a calmer, more confident workforce.
Targeted Screening – Early Detection Saves Lives
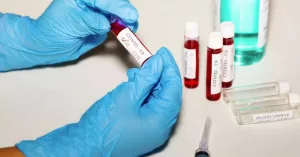
Screening is the “early warning system” that lets us catch infections before they spread. In high‑traffic facilities, routine respiratory virus screening on admission can slash outbreak sizes by up to 30 %—a figure highlighted in several CDC case studies.
When it comes to COVID‑19 testing, the landscape keeps shifting. During periods of high community transmission, weekly testing of staff plus symptom‑triggered testing for patients is a solid strategy. Rapid antigen tests provide results in 15 minutes, while PCR offers greater sensitivity. Choose the method that balances speed, cost, and the level of risk you can tolerate.
For many facilities, the nasal swab test is the workhorse. It’s comfortable enough for repeated use and can detect a broad panel of viruses when paired with multiplex PCR platforms. If you’re wondering whether a nasal swab can replace a more invasive throat swab, the answer is often yes—especially for influenza and SARS‑CoV‑2 detection.
High‑Risk Settings
Not all care environments face the same level of threat. High‑risk settings—such as intensive care units (ICUs), long‑term care facilities, and emergency departments—require extra vigilance.
| Setting | Key Actions | Example Tool |
|---|---|---|
| Acute Care (ICU, ED) | Daily environmental cleaning audits, rapid point‑of‑care testing | CDC “Core Practices” checklist |
| Long‑Term Care | Cohort staffing, visitor screening, vaccination drives | NHMRC 2019 guidelines for care homes |
| Outpatient Clinics | Pre‑visit symptom questionnaires, isolation rooms for symptomatic patients | Standardized triage flowchart |
| Home & Community Care | Portable PPE kits, tele‑health check‑ins, rapid test kits for visits | Public Health Ontario quick‑reference guide |
Each of these environments benefits from a tailored “infection prevention bundle.” In a 2023 outbreak at a mid‑size nursing home, the bundle—consisting of weekly nasal swab testing, enhanced hand‑hygiene audits, and visitor temperature checks—reduced secondary cases by 45 % within two weeks. Real‑world evidence like that makes the abstract guidelines feel tangible.
Balancing Benefits & Risks
Every infection prevention measure comes with a trade‑off. Let’s weigh the scales.
- Benefits: Lower transmission rates, reduced length of stay, cost savings, improved staff morale, and higher patient satisfaction scores.
- Risks: PPE fatigue, false‑negative test results, increased workload, and potential for “alert fatigue” if alerts are too frequent.
Mitigation starts with open communication. Share the why behind each protocol, involve frontline staff in decision‑making, and celebrate small wins—like a week with zero new HAIs. When people understand that a mask isn’t just a policy but a shield for their loved ones, adherence climbs.
Implementation Checklist
Ready to turn knowledge into action? Below is a ready‑to‑use checklist you can paste onto a whiteboard or embed in your quality‑improvement software.
| ✔️ Step | Description | Owner | Frequency |
|---|---|---|---|
| 1 | Hand‑hygiene audit (spot‑check compliance, post results) | Infection Preventionist | Weekly |
| 2 | Respiratory screening protocol (nasal swab on admission) | Admission Nurse | Every admission |
| 3 | PPE stock review (30‑day supply verification) | Supply Manager | Monthly |
| 4 | Education sprint (5‑minute huddle on latest variant updates) | Unit Leader | Bi‑weekly |
| 5 | Data dashboard (track HAIs, test positivity, compliance metrics) | Quality Team | Real‑time |
Feel free to tweak the checklist—add a column for “Notes” or adapt the frequency to fit your staffing model. The goal is to make it a living document, not a static poster.
Resources & Reading
When you want to dive deeper, these trusted sources can serve as your reference library:
- CDC – Infection Control Basics
- NHMRC – Australian Guidelines for Prevention & Control of Infection (2019)
- Public Health Ontario – IPAC quick‑reference guide for home and community care
- Health Quality Innovation Network – Infection Prevention Program Guide
Each of these resources is grounded in rigorous research and updated regularly, so you can be confident that you’re following the most current best practices.
Conclusion
Infection prevention isn’t a single superhero move; it’s a collection of everyday habits, targeted screenings, and thoughtful policies that together create a fortress of safety. By embracing standard and transmission‑based precautions, implementing regular respiratory virus screening and COVID‑19 testing, and tailoring bundles for high‑risk settings, you’ll see fewer HAIs, happier patients, and a more resilient staff.
Take the checklist, share the key points with your team, and consider starting a quick “infection‑prevention huddle” at the beginning of each shift. Small, consistent actions add up to a massive impact. If you’ve tried any of these strategies or have questions about adapting them to your unit, feel free to reach out—let’s keep the conversation going and keep our workplaces safe together.



















Leave a Reply
You must be logged in to post a comment.