Hey there, friend. If you’ve just heard the term “Hepatitis C genotype” and feel a little lost, you’re not alone. In a nutshell, Hepatitis C comes in seven genetic versions—called genotypes. Knowing which one you have guides your doctor toward the right medicines and tells you a bit about how your liver might behave over time. Let’s dive in together, break down the science, and turn those medical terms into something you can actually use.
What Is a Genotype?
Definition and Basics
A genotype is simply a label for the genetic makeup of the Hepatitis C virus (HCV) you’re carrying. Think of it like a fingerprint: each genotype – from 1 to 7 – has a distinctive pattern in the virus’s RNA code. These patterns are called “genotypes,” while the smaller variations within each (like 1a, 1b, 2a) are “sub‑types,” and the tiny twists that happen inside a single person are “quasispecies.” According to Wikipedia, the virus’s rapid replication creates a constantly shifting genetic landscape, which is why these categories matter.
Numbers and Types
There are seven major Hepatitis C genotypes and more than 67 identified sub‑types. The most common worldwide are genotypes 1, 2, and 3. In the United States, genotype 1 dominates, accounting for roughly 75 % of infections, while genotypes 2 and 3 make up most of the rest. Meanwhile, genotype 4 shows up frequently in Africa and the Middle East, genotype 5 is almost exclusive to South Africa, and genotype 6 pops up across Southeast Asia. The newest research even hints at an eighth genotype, but for everyday practice those seven are the big players.
Why Genotypes Matter
Treatment Impact
Here’s where the rubber meets the road. Not all treatments work equally well on every genotype. Some older drugs were genotype‑specific, meaning you needed a different cocktail for genotype 1 versus genotype 2. Today, many of the direct‑acting antivirals (DAAs) are “pangenotypic,” meaning they can clear almost any HCV strain. Still, certain genotypes—especially genotype 1b and genotype 3—may need longer courses or a little extra help from ribavirin. The Treatment Action Group notes that genotype 3 can be a tougher nut to crack, sometimes requiring extended therapy.
Disease Progression Risks
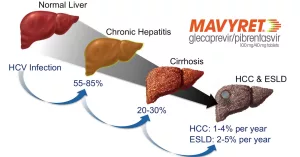
While every genotype can cause liver inflammation, research shows subtle differences in how fast the disease can progress. For instance, genotype 3 has been linked to a quicker march toward fibrosis and cirrhosis, especially if you also have metabolic risk factors like fatty liver. Genotype 1b, on the other hand, appears to carry a slightly higher risk of liver cancer. Knowing your genotype helps your doctor decide how closely to monitor you with imaging and blood tests.
Public‑Health Perspective
Understanding genotype distribution also guides public‑health strategies. If you live in a region where genotype 4 is prevalent, screening programs might focus on different risk groups than a region where genotype 1 dominates. According to CDC data, the global spread of genotypes reflects historic travel, migration, and injection‑drug‑use patterns. That’s why a simple blood test can tell a larger story about community health.
How Testing Works
From Blood to Results
Getting your genotype nailed down is a relatively quick lab process. Your doctor will draw a small blood sample, send it to a certified lab, and the lab will use polymerase chain reaction (PCR) or next‑generation sequencing to read the virus’s RNA. The result comes back as “Genotype 1a” or “Genotype 3b,” for example. The VA’s patient guide explains that the test usually takes a few days, and the report includes any mixed‑infection information if more than one genotype is present.
Mixed Infections
Ever wonder why some people get “mixed infection” results? It happens when a person contracts more than one strain—say, through a blood transfusion that wasn’t screened thoroughly. Mixed infections are rare but can complicate treatment decisions because each genotype may respond differently to the chosen drugs. If you’re in a high‑risk group, your clinician might order a more detailed assay to catch any hidden strains.
Real‑World Example
Take Sam, a 42‑year‑old who received a blood product overseas in the ’90s. When he finally got tested, his lab report read “Genotype 1a + Genotype 3a.” Because genotype 3 can speed up fibrosis, his liver specialist opted for a 12‑week pangenotypic regimen with an extra ribavirin boost. Within three months, Sam’s viral load was undetectable, and his liver elastography showed improvement. Stories like Sam’s illustrate why a precise genotype check isn’t just academic— it can shape the cure timeline.
Genotype Quick Guide
| Genotype | Common Regions | Typical Treatment (2024) | Risk Notes |
|---|---|---|---|
| 1 (1a, 1b) | US, Europe, Japan | Pangenotypic DAAs (sofosbuvir/velpatasvir) – 12 weeks | Higher cirrhosis risk with 1b; generally good response |
| 2 (2a, 2b) | Europe, Japan | Glecaprevir/pibrentasvir – 8‑12 weeks | Usually milder liver disease |
| 3 (3a, 3b) | South‑East Asia, Australia | SOF/VEL + ribavirin or extended DAA course | Faster fibrosis; watch for steatosis |
| 4 (4a‑4d) | Middle East, Africa | Pangenotypic regimen – 12 weeks | Emerging in Europe among PWID |
| 5 (5a) | South Africa | SOF/VEL – 12 weeks | Rare, limited data |
| 6 (6a‑6e) | Vietnam, Hong Kong, Australia | SOF/VEL – 12 weeks | Less studied, but pangenotypic works |
| 7 | Very limited reports | Experimental trials; consult specialist | Rare, unknown long‑term impact |
This table gives you a snapshot of where each genotype lives, which drugs usually work, and any particular red flags. If you ever need to reference it for a doctor’s appointment, it’s a handy cheat sheet.
Symptoms Across Genotypes
Do Symptoms Vary?
Good news: most Hepatitis C symptoms look the same no matter the genotype. Early infection can be silent—many people feel perfectly fine. When symptoms do appear, they often include fatigue, mild jaundice, dark urine, or abdominal discomfort. However, studies suggest genotype 3 may cause liver damage faster, which sometimes translates into earlier onset of “Hepatitis C symptoms” like swelling in the legs (edema) or a more pronounced fatigue.
When to Get Checked
If you notice persistent tiredness, unexplained weight loss, or right‑upper‑abdominal pain, it’s time to talk to a clinician. Blood work (ALT/AST levels) and a FibroScan can gauge liver health. Knowing your genotype adds an extra layer: for genotype 3, doctors might order a FibroScan sooner, given its propensity for quicker fibrosis.
Monitoring Tools
Beyond the basic labs, viral load testing (HCV RNA) tells you whether the virus is still active. After treatment, a “sustained virologic response” (SVR) at 12 weeks post‑therapy means you’re cured. For high‑risk genotypes, ongoing surveillance for hepatocellular carcinoma is advisable, especially if you have cirrhosis.
Living After Diagnosis
Universal Lifestyle Tips
Regardless of genotype, a liver‑friendly lifestyle boosts your odds of a smooth cure. Cut alcohol, stay hydrated, eat a balanced diet rich in antioxidants, and keep a healthy weight. Regular exercise helps, too—just avoid over‑exertion if you have advanced fibrosis.
Genotype‑Specific Follow‑Up
If you’re genotype 1b, your hepatologist may schedule liver imaging every six months after cure because of the slightly higher liver‑cancer risk. For genotype 3, more frequent FibroScans (perhaps every 12 months) can catch any early scarring. The key is open communication: ask your doctor why a particular schedule is recommended.
Support Networks
You don’t have to walk this road alone. Organizations like the Hepatitis C Trust run peer‑support groups where you can swap stories, ask questions, and find encouragement. Connecting with someone who’s already triumphed over genotype 3 can be especially empowering.
Key Takeaways
Quick Checklist
✔️ Get a genotype test as soon as you’re diagnosed.
✔️ Review the recommended DAA regimen; many are pangenotypic, but some genotypes need tweaks.
✔️ Schedule liver health monitoring based on your specific genotype.
✔️ Adopt liver‑friendly habits—no alcohol, balanced diet, regular check‑ups.
✔️ Lean on community resources for emotional support.
Final Thoughts
Understanding Hepatitis C genotypes feels a bit like decoding a secret code—once you know what the letters mean, you can turn that knowledge into action. The science has come a long way: from genotype‑specific, hard‑to‑tolerate interferon regimens to short, well‑tolerated oral pills that clear the virus in over 95 % of cases. Your genotype is a piece of the puzzle, not the whole picture, but it tells you which pieces fit best.
If you’ve just learned you have genotype 1, genotype 3, or any other type, breathe easy. Modern medicine is on your side, and armed with the right information, you can steer your treatment toward a cure. Have questions about your own genotype? Drop a comment below or reach out to a trusted liver specialist—you deserve answers that feel personal, not just clinical.






















Leave a Reply
You must be logged in to post a comment.