Let’s cut to the chase: When you picture someone struggling with osteoarthritis, you might imagine stiffness or sore mornings getting out of bed. But here’s the surprise twist—what’s actually breaking things down faster could be hiding in your pantry or kitchen cabinets.
Yep, malnutrition.
If you’re nodding along because your joints hurt and you’ve been skipping meals or falling back on processed snacks for days, you’re not alone. A 2025 University of Alberta study dropped a truth bomb: folks with both obesity and OA are getting hit with silent nutritional threats. We’re not just talking about a few missed vitamins. These hidden deficiencies mix with inflammation like pouring gasoline on a fire.
Circular Pain: OA and Malnutrition Playing Tag
“How Does Sore Knees Cause Hunger?”
You probably know OA for chewing up your joints—slow grind, thank-you-very-much—but did you ever think it might be quietly messing with your dinner plate too?
Here’s the weird cycle no one talks about: the pain and limited movement from OA make it harder to cook healthy meals. But when you end up living off soggy sandwiches and canned pasta, your body starts screaming even louder through worsening joint damage. It’s mutual destruction—but not in a thrilling way, more like two bullies at a schoolyard who high-five every time you try to handle your arthritis.
Take Sarah’s story, for example. She’s in her early 60s and loves mexican cabbage but stopped eating it because cutting it up for more than a minute twisted her wrist too bad. So, guess what? Her go-to night stir fry turned into bland white bread soup. You can imagine what that did to her inflammation rollercosters—it wasn’t pretty.
When Your Body Starves and Your Doctor Doesn’t Notice
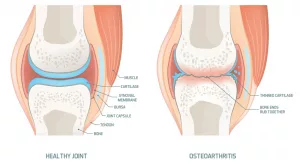
This isn’t weakly expressed concern. Malnutrition straight-up weakens cartilage, especially if protein is off-missing. Ever jot down your inflammation patterns in a chart? Let’s say you’re already doing that. What you’re probably not tracking: how many grams of protein your breakfast smoothie actually has.
A recent analysis in Osteoarthritis and Cartilage explained that protein starvation isn’t just about tired muscles—it rewires your cartilage, making it soft and brittle, like mostly baked bread. Yep, your joints might be silently pleading for more lentils or whoa-gurt—no joke.
And while we’re on bad charts, take a peek at these:
- Low vitamin D = creakier mornings.
- Minus enough omega-3s = stiffer knees.
- Micronutrient gaps = fake reminder to your body: “Prepare for more swelling!”
So, what do you eat these days? Just wondering, because it may matter more than your supplement labels let on.
The Ugly Truth About Fast Weight Loss
“I Dropped 30 lbs—Now My Joints Froze” —Stop That
Hold on—we’re not telling you to stop losing weight if your doctor says it could help. But caution tape needs to go up around quick-and-dirty weight loss plans. Especially if you’re already dealing with OA and age likes to tag-team them.
A 2025 paper in ScienceDirect gave a heads-up: If your calorie-cutting method forgets to support muscle strength or deliver necessary nutrition, weight loss brings something extra to the table — worsened OA progressions.
Let that sink deeper: not all weight loss is healing for your joints, unless you go steady. Otherwise, you’re spending effort to melt fat, while your joints cry out “please, not the muscles nearby!”
The Balanced Way (Yes, There Is One)
Here’s where we turn around and say: “Before you embark on that 7-day detox thing off your phone feed—listen up.”
If your joint pain makes lifting grocery bags hard, or using knives tricky, the solution isn’t just “eat fewer calories.” Your interface with healthy eating is strained already (pun very much intended), so you’ve got to make this smooth. Try these foundational hacks:
- Boost protein first before cutting fats/sugars hard.
- Shake, don’t cook — protein smoothies are a savior if meals feel slow or tricky.
- Swap frozen processed stuff for frozen steamed veg or canned beans—less effort, more nutrition.
Trust us—food that doesn’t sabotage your joints is totally doable (and maybe even delicious) without reinventing your whole kitchen setup.
Doctors Still Miss This? Actually, Yes
No Standard Checks = Major Blindspot
No joke—many specialists still focus their entire OA strategy on the drugs and PT, without diving into your daily bites. Which is real messy because, like I just spilled earlier, protein matters and sometimes weird deficiencies are behind your joint cries.
Let’s Compare Standards
| To-do at Appointments | Mission-Control Neglect |
| asking about pain levels | ❌ no nutrition assessment |
| examining swelling | ❌ ignoring fiber or protein intake |
| tracking mobility | ❌ skipping food insecurity check |
If you’ve ever left the clinic wondering, “But what about my tired legs or why my body feels like windpaper?”—now you know part of the gap. Malnutrition can mirror OA progression but fly under everyone’s radar—and leave you going around in circles of pain.
What Experts Are Debating Right Now
We’re still parsing things like “What’s ideal vitamin D level for OA progression?” or “Should omega-3 guidelines act like flexible rules or mandatory ones?”
According to OARSI 2024 talks, there’s still a lot to agree on. No single “diet plan” hits all cases. Some folks see changes when they go Mediterranean-style; others find relief with tweaky fat adjustments they swear by. We don’t have a final manual yet… but we do have a pretty good start to map what prevents your health from snowballing.
Simple Moves to Start Reversing the Cycle
Good Foods That Don’t Require Basic Knife Skills
Let’s say your wrists or your morning stiffness doesn’t make chopping worthwhile. There’s still hope. Swap obviously suspect stuff for smarter choices that travel at you with more nutrition than hassle:
- Pre-cut frozen vegetables or canned ones? Yep, they count. You’re not required to peel EVERYTHING.
- Eggs for days — besides being protein kings, they can be scrambled, steamed, boiled… all joint-friendly techniques.
- Canned beans instead of dry? Perfect for soups and grabs way more micronutrients.
The point? This doesn’t need a chef’s hat at the start.
When to Call Nutritional Back-Up
Your doctor probably doesn’t have time to spill on your carbs. That’s where a nutrition pro comes in. A point they bring up early is coaxing out early signs:
- Brittle nails or dry skin
- Weaker sleep or fading muscle strength
Those might sound like weak topics, but in OA folks, they show malnutrition clawing at areas you didn’t expect yet.
Ask for a nutritionist friend squad member early. Sometimes easing your symptoms is rearranging your plate, not just your radiology report.
OA Isn’t Just About Wear-and-Tear
Getting Past the Mechanical Excuses
Okay—someone out there is tired of hearing “OA is just aging” stuff. But listen. On top of physical breakdowns, OA also brings emotional rhythm too fast for calm nights. World Health Organization doesn’t label OA as just a joint driver. It cuts your quality of life—shops you off walking, reading, even sitting comfortably for Sunday coffee. One guy we talked to put it best: “if you make light choices too long, one day your plants die—that’s your independence saying hi.”
Only the small wins matter at first. It’s similar to cleaning a spot, not overhauling the bathroom with suds in the first week. Just add peas next week. That’s movement.
Short-Term Fix, Long-Term Problem
Your favorite cheat food might be the only one that soothes a sciatic nerve flare-up right now. We get it. But here’s the handoff: when you live in survival mode over months (which OA does reliably ask for), even the thing that calms you in the hour might kick-start a longer issue like stronger nutritional imbalances or higher inflammation.
This isn’t about being “good.” It’s about how consistent food can add support, even when your joints are not feeling cooperative. Malnutrition isn’t a “one misstep.” It’s sneaky and steady—like a wrong pillow that latently messes with your neck days.
Where Do You Go From Here?
At the start, this wasn’t about calling rocks out-of-place. It was about showing that over time, nutrition shifts have silent power that’s been underestimated in crippling OA pain. The next step isn’t perfection—even minor shifts act as reset buttons.
- Refusing to brush off bone pain again as “just loading”
- Lean into protein sources that work with you, not armies of knives
- Speak to someone beside your PT or doctor, maybe someone who speaks in substrate and “deficiencies,” instead of “damage” or “degeneration”
- Prepare if not now—just track what’s missing in your meals
There’s no final arthritis cure yet, but fights can get better when microshifts pump nutrition into the joint space. And if you’re interested, we can dive into the nuts and bolts that predict OA nutritional patterns, a study by Osteoarthritis Research Society International back in 2024 started breaking these down deeply.
So—what’s one thing you’re already doing that could shift next week? We’re curious what you’ve found sneaks onto your plate! Share your stories or tricky days.

















Leave a Reply
You must be logged in to post a comment.