Quick Answer
Malnutrition can knock the wind out of anyone’s day‑to‑day enjoyment. It drags down physical stamina, clouds mental sharpness, and isolates people from the activities they love. In older adults and people living with chronic diseases, the hit to quality of life is often measured in a 15‑20 % drop on standard health‑related questionnaires. In short, if you’re not getting enough nutrients, your overall wellbeing suffers – fast.
Core Concepts
What Is Malnutrition?
Most of us think malnutrition only means “not enough food,” but medically it’s any imbalance of nutrients – too little protein, missing vitamins, or even excess calories paired with hidden deficiencies. The gold‑standard tools for spotting it in a clinic are the Mini‑Nutritional Assessment (MNA) and the Patient‑Generated Subjective Global Assessment (PG‑SGA). Both look at weight changes, food intake, and functional status.
| Tool | Key Items | Score Range | Interpretation |
|---|---|---|---|
| MNA | Appetite, weight loss, BMI, calf circumference, disease impact | 0‑30 | ≥24 = well‑nourished; 17‑23.5 = at risk; <17 = malnourished |
| PG‑SGA | Weight loss, intake change, symptoms, activity, disease | 0‑9+ | 0‑3 = well‑nourished; 4‑8 = moderately malnourished; >9 = severe |
What Does “Quality of Life” Mean?
Health‑related quality of life (HRQoL) is a fancy way of saying “how good you feel while you’re alive.” Researchers capture it with surveys like the SF‑36, EQ‑5D, or the cancer‑specific EORTC QLQ‑C30. These tools break wellbeing into four domains: physical function, mental health, social participation, and symptom burden.
Why Is It a Two‑Way Street?
Think of malnutrition and QoL as a tug‑of‑war rope. Poor nutrition weakens muscles, lowers immunity, and fuels fatigue, which in turn makes it harder to prepare healthy meals or stay active. Conversely, when a person feels depressed, isolated, or in pain, they often eat less, spiralling the deficiency further.
Who’s Most at Risk?
- Older adults (especially ≥ 65 years)
- People with heart failure or chronic kidney disease
- Cancer patients undergoing chemo or radiation
- Individuals battling osteoarthritis or severe joint pain
- Those living with obesity yet experiencing micronutrient gaps – the “obesity‑malnutrition paradox”
For a deeper dive into the obesity side of things, check out our piece on obesity and malnutrition.
Condition Impacts
Heart Failure
Advanced heart failure patients often lose appetite because of fluid overload and medication side effects. A cohort study that examined patients with “malnutrition quality of life” found that malnourished individuals reported a 30 % higher rate of hospital readmission and markedly lower scores on daily‑living questionnaires. In plain English: they felt weaker, more short‑of‑breath, and less able to care for themselves.
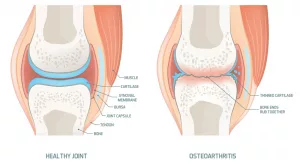
Osteoarthritis
Joint pain can make chewing painful, especially when dentures don’t fit right. Poor oral health, in turn, reduces food variety and pushes people toward soft, nutrient‑poor meals. This hidden loop is explored in our article on osteoarthritis hidden factors. Studies also link low vitamin D and omega‑3 intake to higher pain scores, meaning better nutrition can actually ease the ache.
Cancer & Dialysis
Imagine undergoing dialysis three times a week while battling nausea. The British Journal of Nutrition reported that dialysis patients with protein‑energy malnutrition scored 20 % lower on the SF‑36 physical component. Similarly, a large gastric‑cancer cohort (4,586 participants) showed that patients with a PG‑SGA ≥ 4 had dramatically reduced global QoL scores, especially in appetite and fatigue domains.
Obesity‑Related Sarcopenia
Yes, you can be both overweight and under‑nourished. Excess fat masks muscle loss, leading to “sarcopenic obesity.” Those individuals often feel exhausted after climbing a single flight of stairs, a classic sign that their quality of life is suffering despite a higher body weight.
HIV & Chronic Illness
A 2015 study from Nepal found that people living with HIV who scored low on the MNA also reported poorer mental health and lower social functioning. The pattern repeats across many chronic conditions: the worse the nutrition, the lower the QoL.
Screening & Assessment
Routine Primary‑Care Checks
Every annual visit for anyone over 65 should include an MNA. It takes five minutes, costs nothing, and flags problems before they snowball. If the score lands below 17, a deeper nutritional work‑up is warranted.
Pairing With QoL Surveys
Combine the MNA with the SF‑36 or EQ‑5D to get a full picture. The two together reveal whether low scores stem from physical weakness, mental distress, or both.
Red‑Flag Indicators
- Unintentional weight loss > 5 % in three months
- Serum albumin < 3.5 g/dL
- Depression questionnaire score > 10
- Severe pain interfering with meals
Community Interventions
Home‑visiting nurses who deliver fortified meals and monitor intake have cut malnutrition rates by 12 % in a recent Innovation in Aging pilot. Such programs also boost patients’ confidence in managing their own health.
For more on how osteoarthritis ties into nutrition, see our guide on Malnutrition and osteoarthritis.
Nutrition Strategies
Protein‑Rich, Energy‑Dense Meals
Aim for 1.2–1.5 g of protein per kilogram of body weight each day, plus 30–35 kcal per kilogram for total energy. Think Greek yogurt topped with nuts, lean turkey wraps, or a hearty lentil stew – foods that pack both protein and calories without a massive bulk.
Micronutrient Optimization
- Vitamin D: 800–1,000 IU daily (especially for bone‑health and joint pain)
- Calcium: 1,200 mg for adults over 50
- Omega‑3 fatty acids: 1–2 g EPA/DHA from fish or supplements
- B‑complex vitamins: crucial for energy metabolism
Condition‑Specific Diet Tweaks
| Condition | Key Dietary Focus | Why It Helps |
|---|---|---|
| Heart Failure | Low sodium, adequate potassium, moderate protein | Reduces fluid retention, supports heart muscle |
| Osteoarthritis | Anti‑inflammatory foods (olive oil, fatty fish), calcium, vitamin D | May lower joint inflammation and preserve cartilage |
| HIV | High‑protein, high‑calorie, micronutrient‑dense | Fights opportunistic infections and muscle loss |
| Dialysis | Controlled phosphorus, high‑quality protein, fluid management | Prevents mineral imbalance while preserving muscle |
Physical Activity + Nutrition
Resistance training two to three times a week, paired with a post‑workout protein snack (like a whey shake or cottage cheese), can reverse muscle loss within eight weeks. Your body will thank you with higher energy levels and a brighter mood.
Psychosocial Support
Depression, anxiety, and social isolation often accompany malnutrition. Simple steps—regular phone check‑ins, meal‑prep buddies, or community cooking classes—can lift spirits and encourage better eating habits.
Real‑World Stories
Mrs. López’s Turnaround
Mrs. López, a 78‑year‑old with congestive heart failure, arrived at her clinic with an MNA of 7 and a drab SF‑36 physical score of 32. A home‑visit dietitian introduced a 1,200‑kilocalorie, high‑protein plan and set up weekly telephone coaching. Six months later, her MNA rose to 13, she regained 5 kg of lean mass, and her physical QoL jumped to 58. “I feel like I can finally enjoy my garden again,” she told us, eyes sparkling.
Mr. Chen’s Cancer Journey
Mr. Chen, 62, was diagnosed with gastric cancer and scored a 9 on the PG‑SGA, indicating severe malnutrition. After a multidisciplinary nutrition program—tube‑feeding, vitamin D supplementation, and counseling—his PG‑SGA dropped to 4. His global QoL score on the EORTC QLQ‑C30 rose from 44 to 71, and he reported being able to “laugh at jokes again” during chemotherapy.
Community Success in Jakarta
A school‑based nutrition initiative in Jakarta screened 200 children for malnutrition using the MNA. Those identified received fortified milk and nutrition education. By the end of the year, PedsQL scores (a child‑focused QoL measure) improved by an average of 12 points, reflecting better health, mood, and school performance.
Take Action Today
Understanding that malnutrition isn’t just “not eating enough” is the first step toward reclaiming a vibrant life. If any of the red‑flags above sound familiar, consider asking your doctor for an MNA screening. Even a simple change—adding a protein‑rich snack after a walk—can start shifting the balance toward better health.
Ready to explore more? Read about the hidden nutritional triggers of joint pain in our article on osteoarthritis health risks. And if you’re curious how weight, muscle, and nutrients interact, our deep dive on obesity and malnutrition offers practical tips.
Remember, you don’t have to navigate this alone. Nutritionists, nurses, and supportive friends are all part of the team that can help you boost your quality of life. Take that first step today—schedule a screening, add a nourishing food, or simply share what you’ve learned with someone who might need it.

















Leave a Reply
You must be logged in to post a comment.