Ever wonder why your knees ache even though you haven’t slammed a weight on them or why your hands feel stiff despite never doing heavy labor? It’s not always about age or obvious wear‑and‑tear. A bundle of “hidden” influences—diet, gut microbes, subtle hormone shifts, and silent immune activity—can be pulling the strings behind osteoarthritis. In the next few minutes we’ll walk through those secret drivers, show you how to spot them, and give you practical steps to keep your joints happy. Grab a cup of tea, settle in, and let’s uncover what you might have missed.
Why Hidden Matters
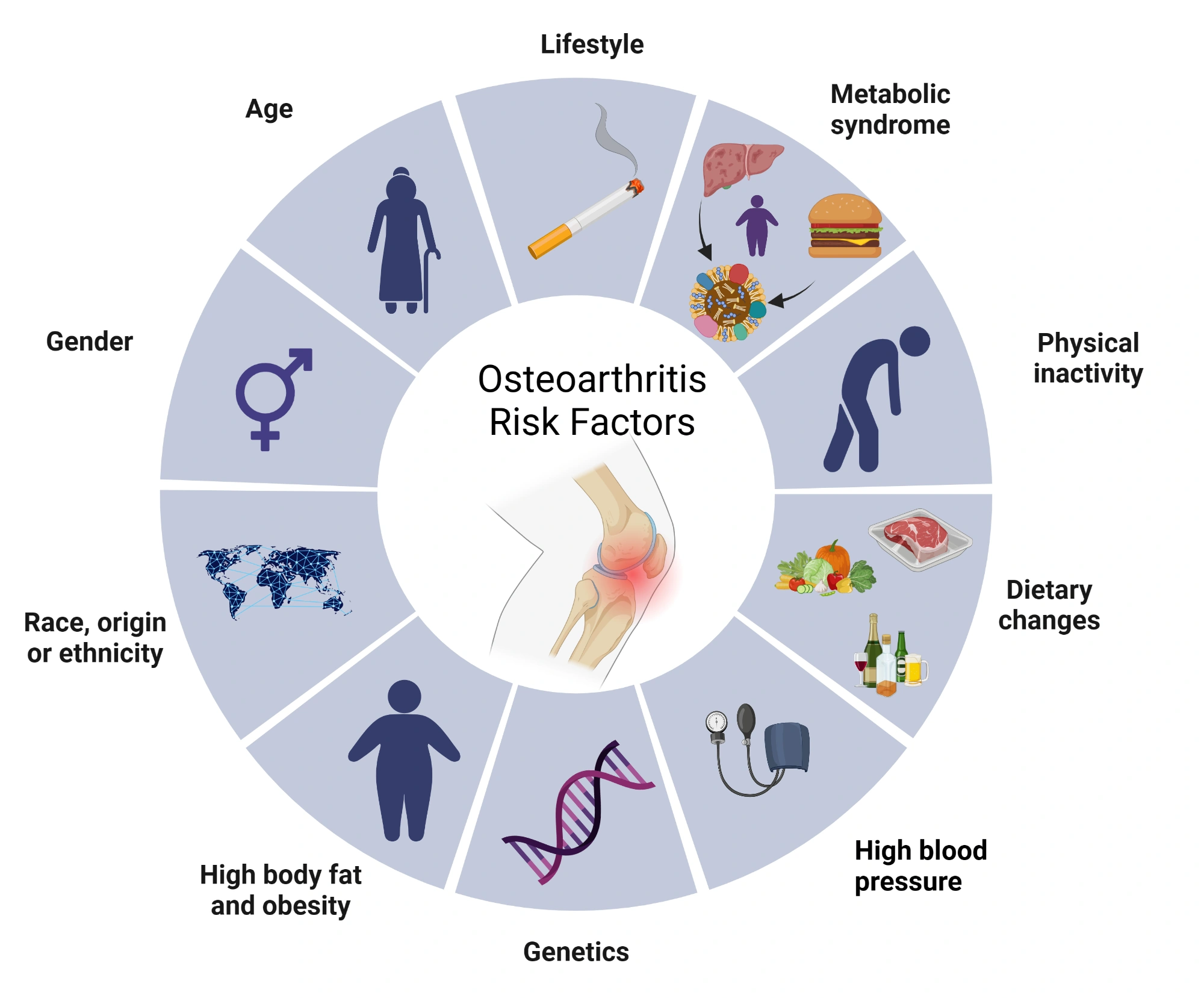
When we talk about osteoarthritis, most people picture an old body that’s simply “used up.” The classic line is: age plus weight equals joint pain. But recent research tells a richer story. A 2022 article from Warner Orthopedics emphasizes that osteoarthritis (OA) is fundamentally inflammatory, not just mechanical wear. That means the damage can start long before you feel any creak or groan in your joints.
So why do these hidden factors matter? Because they’re modifiable. If you can tweak your diet, balance your hormones, or nurture your gut, you may slow—or even reverse—joint degeneration. Think of it like fixing a leaky pipe before the ceiling collapses; the sooner you attend to the source, the less damage you’ll see later.
Nutrition & Metabolism
Most of us hear the phrase “obesity is a risk factor for OA,” but what about the other side of the nutritional coin—malnutrition? It turns out both extremes can sabotage joint health.
Obesity vs. Malnutrition – Why Both Hurt Joints
Excess body fat releases cytokines—tiny inflammatory messengers—that fan the flames of cartilage breakdown. At the same time, a lack of essential nutrients starves chondrocytes (the cells that build cartilage) of the building blocks they need. A study in Frontiers in Aging showed that low‑grade inflammation in the gut, driven by poor diet, can accelerate cartilage loss.
For a real‑world picture, check out this piece on obesity and malnutrition. It explains how a diet high in refined carbs and low in micronutrients creates a perfect storm for joint inflammation.
Key Micronutrients That Protect Cartilage
| Micronutrient | Why It Matters | Good Sources |
|---|---|---|
| Vitamin D | Supports bone mineralisation and modulates immune response | Fatty fish, fortified dairy, sunlight |
| Omega‑3 Fatty Acids | Reduces inflammatory cytokines (e.g., IL‑6) | Salmon, walnuts, flaxseed |
| Collagen‑Peptides | Supplies amino acids for cartilage matrix | Bone broth, hydrolysed collagen supplements |
| Magnesium | Essential for collagen synthesis and nerve function | Dark leafy greens, almonds, pumpkin seeds |
| Vitamin C | Antioxidant that protects cartilage from oxidative stress | Citrus, berries, bell peppers |
Even a modest deficiency can tip the balance toward degeneration. If you suspect you’re not getting enough, consider a simple blood test or a conversation with your dietitian.
Malnutrition’s Impact on Quality of Life & OA Progression
When the body lacks nutrients, the cartilage matrix becomes brittle, and pain spikes. The connection between poor nutrition and lower malnutrition quality of life is striking—people report higher pain scores, reduced mobility, and a faster march toward joint replacement.
Practical “Food‑Swap” Checklist
- Swap sugary cereals for Greek yogurt topped with berries.
- Replace fried potatoes with roasted sweet potatoes (more beta‑carotene, less omega‑6).
- Trade white bread for whole‑grain sourdough (supports gut microbiota).
- Use olive oil sparingly and choose avocado oil for high‑heat cooking.
- Include a daily probiotic‑rich food—think kefir or fermented veggies.
Small changes add up, and you’ll notice less joint stiffness within weeks.
Immune & Hormone Triggers
Beyond what you eat, the immune system and hormones can play sneaky roles in joint health.
Mast Cells – The “Unknown” Culprits
Stanford researchers discovered that mast cells—immune cells best known for allergic reactions—release enzymes that directly erode cartilage. In mouse models, eliminating mast cells entirely stopped osteoarthritis from developing, even when the joints were physically stressed. The study, reported in Stanford’s mast‑cell breakthrough, suggests that chronic low‑grade allergies could be silently damaging your joints.
Do you often experience unexplained itching, sinus congestion, or occasional hives? Those could be clues that mast‑cell activity is high. Talking to an allergist or an immunologist might uncover an unexpected treatment path.
Hyper‑Thyroidism and OA Risk in Seniors
A 2024 Nature study examined more than 7,000 people and found that hyper‑thyroidism more than doubled the odds of developing osteoarthritis in the 60‑80 age group (OR ≈ 2.86). The researchers used Mendelian randomisation to confirm a causal link, meaning the hormone imbalance itself—not just lifestyle—can aggravate cartilage wear.
If you’re over 60 and notice joint pain that doesn’t fit the typical “wear‑and‑tear” pattern, it might be worth checking your thyroid levels. Treating hyper‑thyroidism often improves both metabolic health and joint comfort.
Systemic Inflammation vs. Local Wear‑and‑Tear
Inflammation is the common denominator linking obesity, malnutrition, mast‑cell activation, and thyroid imbalance. The NF‑κB pathway—a master regulator of chronic inflammation—gets turned on by high glucose, excess fatty acids, and even stress hormones. Once activated, it releases catabolic enzymes that nibble away at cartilage.
Ways to calm this fire?
- Eat anti‑inflammatory spices like turmeric (with black pepper for better absorption).
- Practice gentle movement—tai chi, swimming, or a brisk walk.
- Prioritise 7‑9 hours of sleep; poor sleep spikes cortisol, which fuels NF‑κB.
- Manage stress through mindfulness or breathing exercises.
Gut Microbiome Link
Our gut is a bustling metropolis of microbes that communicate with every organ, joints included. When the microbial balance tips toward harmful species, the gut lining becomes leaky, letting endotoxins flood the bloodstream and provoke joint inflammation.
What the Gut‑Microbiota Does for Joints
The 2016 article “Diet‑Intestinal Microbiota Axis in Osteoarthritis” highlighted short‑chain fatty acids (SCFAs) produced by healthy bacteria as protectors of cartilage. SCFAs dampen inflammation and support the synthesis of extracellular matrix proteins.
Hidden Dietary Culprits That Disrupt the Microbiome
Processed snacks, artificial sweeteners, and excessive omega‑6 vegetable oils (like corn or soybean oil) can feed “bad” bacteria and reduce SCFA production. Over time, this creates a low‑grade inflammatory environment that feeds OA.
Probiotic & Prebiotic Strategies
Start simple:
- Morning kefir (½ cup) or a probiotic capsule with at least 10 billion CFU.
- Add a serving of prebiotic fiber—think chicory root, garlic, or a banana—each day.
- Include fermented vegetables (sauerkraut, kimchi) 2‑3 times weekly.
These tweaks help restore a microbiome that whispers “heal” rather than “attack.”
Connecting to Malnutrition and osteoarthritis
Even if you’re not underweight, nutrient‑poor eating can starve both your joints and your gut bacteria. The synergy between malnutrition and a disturbed microbiome amplifies pain and reduces quality of life—something highlighted in the linked article.
Lifestyle & Mechanics
While hidden factors dominate the conversation, we can’t completely ignore mechanics. However, the classic “weight‑plus‑wear” model is only part of the picture.
Why Weight Alone Isn’t Enough
Obese individuals often develop hand osteoarthritis—a joint that isn’t weight‑bearing. This paradox, reported by Jiang 2016, suggests that metabolic inflammation, not just mechanical load, drives joint damage.
Joint Malalignment & Biomechanics
The Rheumatologist’s recent column argues that subtle joint misalignment can amplify stress on cartilage, turning a modest inflammatory environment into full‑blown degeneration. Simple foot‑strengthening or hip‑abductor exercises can correct alignment and relieve pressure.
Exercise That Protects Cartilage
- Quadriceps sets: 3 × 10 seconds, twice daily.
- Hip bridges: 12 reps, 3 sets, 3 times per week.
- Balance board or single‑leg stands: 30 seconds each side.
Low‑impact activities like swimming or cycling keep joints moving without crushing them.
Sleep, Stress & Hormonal Balance
Sleep deprivation raises cortisol, which in turn stimulates NF‑κB—our inflammation bully. A nightly routine that includes dim lighting, a screen‑free hour, and a brief meditation can dramatically improve joint comfort.
Quick Reference Tools
Risk‑Factor Checklist (Downloadable PDF)
When you’re busy, a quick glance at a checklist helps you see where you might be vulnerable. Below is a condensed version you can copy into a note‑taking app.
| Factor | Present? | Action |
|---|---|---|
| High BMI or central obesity | ✔ / ✘ | Mindful eating, regular cardio |
| Micronutrient gaps (Vit D, Mg, Omega‑3) | ✔ / ✘ | Targeted supplements, food swaps |
| Thyroid imbalance | ✔ / ✘ | Blood test, endocrinology consult |
| Frequent allergies / mast‑cell symptoms | ✔ / ✘ | Allergy work‑up, antihistamines |
| Gut dysbiosis signs (bloating, irregularity) | ✔ / ✘ | Probiotic + prebiotic routine |
| Joint misalignment (knee valgus, hip drop) | ✔ / ✘ | Physical‑therapy guided exercises |
Cartilage‑Health Scorecard
Rate yourself from 0 – 10 on each of the following categories (0 = poor, 10 = excellent). Add up the scores; the higher the total, the better your joint odds.
- Nutrition density
- Body composition
- Sleep quality
- Stress level
- Gut health
- Hormonal balance
A score above 45 suggests you’re on the right track; below that, it may be time for a lifestyle audit.
Wrap‑Up
Osteoarthritis isn’t a destiny you have to accept. It’s a complex conversation between your diet, immune system, hormones, gut microbes, and the way you move. By shining a light on the hidden factors—mast‑cell activity, thyroid imbalance, micronutrient shortfalls, and microbiome disruption—you gain real tools to protect your cartilage.
Start small: swap one sugary snack for a probiotic‑rich option, book a thyroid screening if you’re over 60, or add a daily turmeric latte. Those tiny actions compound, creating a joint-friendly environment that lets you stay active, pain‑free, and ready for life’s next adventure.
What hidden factor surprised you the most? Have you already tried any of the food swaps or sleep tricks? Share your thoughts, and let’s keep the conversation going. Your joints— and your future self— will thank you.
For deeper dives, explore these resources: osteoarthritis health risks and the linked articles on nutrition, gut health, and immune triggers.















Leave a Reply
You must be logged in to post a comment.