Experiencing vulvar soreness, itching, or discomfort is fairly common, particularly around the time of your menstrual cycle.
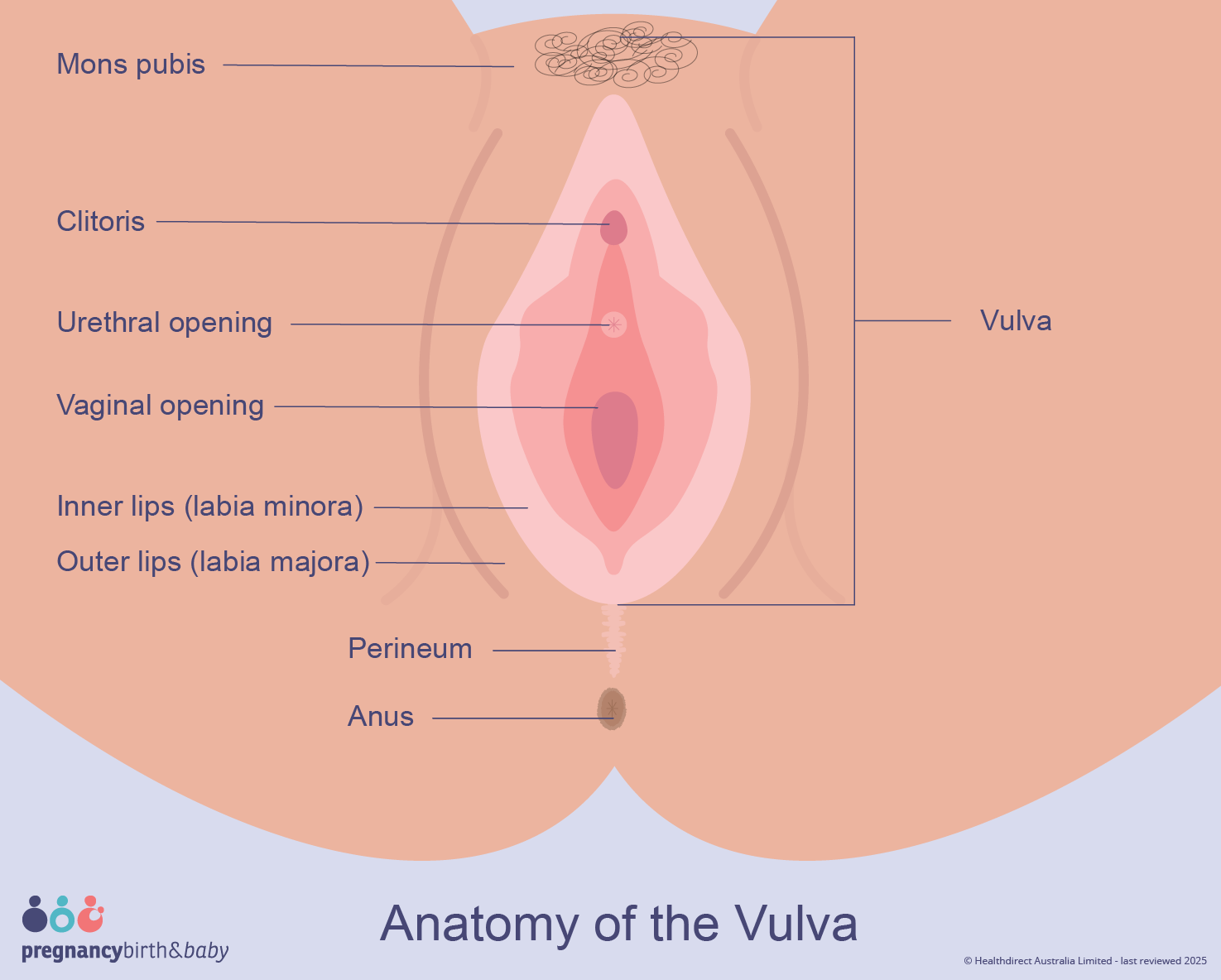
The vulva refers to the external genital structures of people with vaginas. It comprises the outer lips (labia majora) and inner lips (labia minora), plus the pubic mound, the clitoris, and the openings of the urethra and vagina.
This article reviews possible reasons for vulvar pain, how clinicians diagnose them, and what treatments and self-care approaches can help.
Causes of vulvar pain
| Common causes of vulvar pain | Less common causes of vulvar pain |
| vulvodynia | Bartholin’s gland cyst |
| yeast infection | vaginismus |
| bacterial infection | vulvar cancer |
| folliculitis | chronic pain conditions, such as fibromyalgia, interstitial cystitis, or irritable bowel syndrome |
| trichomoniasis |
Vulvodynia
Vulvodynia describes persistent vulvar discomfort, burning, or irritation that lasts for at least three months. It is idiopathic, meaning a clear cause often cannot be identified. Symptoms may occur spontaneously or be triggered by touch.
Cyclic vulvodynia, sometimes called cyclic vulvitis, fluctuates with your menstrual cycle. Pain can intensify around menstruation, particularly when inserting a tampon, though in some individuals symptoms ease during menses.
Although the exact cause of vulvodynia remains unclear, potential contributing factors include:
- prior vaginal infections
- allergic reactions or skin sensitivities
- nerve injury near the vulvar region
- hormonal shifts
- pelvic floor muscle dysfunction
- certain hereditary conditions
Vulvodynia may affect as many as 16 percent of women.
Yeast infection
Roughly 75 percent of women will experience at least one vaginal yeast infection during their lives. It results from an overgrowth of yeast. Possible triggers include:
- hormonal shifts from pregnancy or birth control pills
- antibiotic use or topical antimicrobials
- douching or using harsh feminine care products
- tight or non-breathable underwear or clothing
- poorly controlled diabetes
Symptoms can include pain with urination, discomfort during sex, or pain with tampon insertion, and often a thick white discharge.
Bacterial infection
Bacterial vaginosis occurs when the vaginal pH balance is disrupted. This can follow changes in sexual partners or douching. It may cause foul-smelling discharge and a burning sensation when urinating.
Folliculitis
Folliculitis is inflammation of hair follicles that produces small red bumps, typically on the outer labia.
Bartholin’s gland cyst
A Bartholin’s gland cyst can develop on either side of the vaginal opening when a gland becomes obstructed. A painful cyst often indicates infection.
Trichomoniasis
Trichomoniasis is a common sexually transmitted infection caused by a parasite. Symptoms can include unusual discharge with a strong odor, painful urination, and discomfort with intercourse or tampon use; some people also experience lower abdominal pain.
Vaginismus
Vaginismus involves involuntary, painful spasms of the vaginal muscles. It may occur during sexual activity, pelvic exams, or tampon insertion. Anxiety and a history of sexual trauma are potential contributing factors.
Vulvar cancer
Vulvar cancer is uncommon and slow-growing. Risk factors can include:
- vulvar intraepithelial neoplasia
- human papillomavirus (HPV) infection
- a history of genital warts
Other signs of vulvar cancer may include:
- persistent itching
- bleeding outside of the menstrual period
- changes in skin color or thickness
- lumps, bumps, or sores
Chronic pain conditions
Research from 2012 found that people with vulvodynia are more likely to also have one or more chronic pain syndromes such as:
- fibromyalgia
- interstitial cystitis
- irritable bowel syndrome
Can those in perimenopause and postmenopause experience vulvar pain?
Anyone with a vulva can develop vulvar pain. It’s not unusual for symptoms to begin in midlife or after menopause for many of the same reasons they occur earlier.
Low estrogen levels in perimenopause or after menopause can contribute to vulvar pain. Accompanying signs may include vaginal dryness and vulvar thinning or atrophy.
Medical treatment
Treatment for period-related vulvar pain depends on the underlying cause.
For vulvodynia
Clinicians may treat vulvodynia with topical anesthetics or hormone creams applied to the affected skin. In some cases, certain antidepressants or anticonvulsant medications can reduce symptoms.
For yeast infections
Yeast infections are treated with antifungal agents, many of which are available over the counter as creams, tablets, or suppositories.
If you’ve never been diagnosed with a yeast infection, consult your doctor before using OTC treatments. Antifungal medications won’t help other causes of vulvar pain.
For bacterial infections
Antibiotics are typically used to treat bacterial infections.
Both yeast and bacterial infections should be treated even during menstruation. If you’re using vaginal creams or suppositories for a yeast infection, tampons can reduce the effectiveness of the medication, so consider using pads instead.
For folliculitis
Folliculitis often resolves on its own. A doctor can drain an uncomfortable Bartholin’s gland cyst if necessary. Warm compresses can provide temporary relief.
For trichomoniasis
Trichomoniasis is usually treated with a single oral dose of metronidazole. It’s important that both you and sexual partners receive treatment to prevent reinfection.
For vaginismus
Treatments for vaginismus may include:
- Kegel exercises to strengthen and gain control over pelvic muscles
- use of vaginal dilators to increase flexibility and reduce discomfort
- therapy or counseling with a mental health professional
For vulvar cancer
Treatment options for vulvar cancer can include:
- surgery
- topical medications
- chemotherapy
- biologic therapies
- radiation
Home remedies
If vulvar pain flares during your period, try switching from tampons or menstrual cups to pads to see if that helps. If you already use pads, try changing brands to rule out sensitivity to a particular product.
Other strategies to manage vulvar discomfort include:
- Wearing loose underwear with a breathable cotton crotch.
- Avoiding tight pants or shorts.
- Applying a cold compress or cool gel pack to reduce pain and itching.
- Avoiding activities that press on the vulva, such as cycling or horseback riding, especially during sensitive times.
- Skipping hot baths and hot tubs, which can worsen irritation; instead, take short sitz baths (5 to 10 minutes) several times daily, even while menstruating.
- Avoiding douches, genital deodorants, or fragranced feminine products.
- Using gentle, non-irritating soaps and shampoos.
- Washing the genital area with plain water and gently patting dry.
- After washing, applying plain petroleum jelly or another preservative-free emollient only to external areas.
- Using a lubricant for sex if needed, but avoiding products with alcohol, flavors, or warming/cooling additives.
When to see a doctor
Seek medical care for vulvar pain, especially if you have additional symptoms. Many causes of vulvar pain respond well to treatment, but untreated fungal infections, STIs, and other conditions can cause complications.
You can schedule an appointment with an OB-GYN in your area using our Healthline FindCare tool.
After discussing your symptoms and medical history, your clinician will likely perform a pelvic exam to inspect the area. Swabs of the vagina and vulva can identify bacterial or yeast infections and guide appropriate treatment.
The takeaway
Chronic vulvar pain can significantly impact quality of life, but many causes are treatable.
Whether pain is linked to menstruation or not, consult your doctor if you have vulvar pain. Most causes are manageable, and it’s important to exclude more serious conditions.


















Leave a Reply
You must be logged in to post a comment.