If you or someone you love lives with heart disease, the thought of moving can feel a little scary—like you’re walking a tightrope and don’t want to slip. The good news is that the right kind of movement is actually a proven lifeline, not a hazard. Below you’ll find the quickest, doctor‑approved ways to stay active, lower risk, and keep confidence high without over‑taxing the heart.
These guidelines focus on low‑impact cardio, gentle strength work, and everyday activities that protect the heart while still feeling enjoyable. Let’s jump right into the workouts that really work for older adults dealing with heart disease.
Why Exercise Matters
The heart is a muscle, too
Just like any other muscle, the heart gets stronger when you use it regularly. According to Healthline’s review of exercise for heart disease, consistent movement improves the heart’s pumping ability and keeps arteries flexible, reducing the strain each beat puts on the organ.
Research‑backed benefits
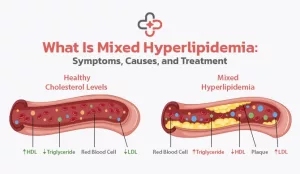
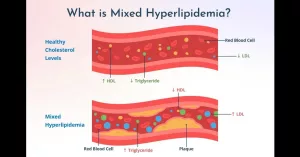
Studies repeatedly show that regular activity does more than just keep you fit—it actually lowers key risk factors. A British Medical Journal analysis found that brisk walking can raise “good” HDL cholesterol and cut coronary events by more than 50 %. Another study cited by the American Heart Association links moderate‑intensity exercise to a 30 % drop in heart‑related mortality.
What happens when you sit still
Too much sitting is a silent killer. The AHA’s journal Circulation estimates that about 250,000 U.S. deaths each year are tied to a sedentary lifestyle. Inactivity raises blood pressure, spikes LDL (“bad”) cholesterol, and makes the heart work harder during everyday tasks.
How much is enough?
The classic guideline is 150 minutes of moderate‑intensity aerobic activity per week (about 30 minutes, five days a week). For seniors, the “talk test” is a handy shortcut: you should be able to hold a conversation, but not sing, while you move. If you can’t talk at all, dial the intensity down.
Core Principles
Medical clearance first
Before you lace up any shoes, check with your doctor. A graded exercise (stress) test helps determine safe heart‑rate zones and uncovers any hidden arrhythmias. Your cardiologist may suggest specific limits based on your diagnosis, medications, and overall fitness.
The “5‑B” framework
Think of these five B’s as your safety net:
- Breathing: Keep a steady rhythm; avoid holding your breath during effort.
- Balance: Choose stable surfaces and supportive footwear.
- Begin‑slow: Start with just a few minutes and add time gradually.
- Build‑gradually: Increase duration or intensity by no more than 10 % each week.
- Back‑off if needed: Stop immediately if you feel dizziness, chest pressure, or unusual shortness of breath.
Watch your intensity
Because many heart medications (like beta‑blockers) blunt your pulse, rely on perceived exertion instead of numbers alone. The Borg Rating of Perceived Exertion (RPE) scale—aim for a 3‑5 out of 10—works well. If you’re unsure, the talk test remains your simplest gauge.
Consistency over intensity
It’s better to move a little every day than to push hard once a week. The heart adapts to regular, moderate stress; occasional spikes can actually increase risk of arrhythmias, especially in older adult fitness programs.
Low‑Impact Cardio
Walking
Mall‑walker technique
Pick a local shopping mall or a safe indoor hallway. Start with a 5‑minute warm‑up (slow stroll), then aim for a steady 20‑minute walk at a pace that lets you talk comfortably. Finish with a 5‑minute cool‑down. A cadence of about 100 steps per minute usually hits the moderate‑intensity sweet spot.
Stationary or Recumbent Cycling
Setting it up
Adjust the seat so your knees are slightly bent at the bottom of the pedal stroke. Begin on resistance level 2‑3 and pedal for 10‑15 minutes, gradually building to 30 minutes. Keep the handlebars within easy reach to avoid straining your shoulders.
Water Aerobics & Swimming
Why it’s gentle
Water supports your joints, reduces impact forces, and naturally cools you down. A 30‑minute water‑aerobics class—think arm circles, leg kicks, and gentle marching in the shallow end—delivers a solid cardio boost without the jarring pounding of land‑based moves.
Dancing & Low‑Impact Aerobics
20‑minute routine
Put on your favorite song and do a simple step‑touch, side‑to‑side, and gentle arm swing pattern. Keep the beats around 100–110 per minute; after a few weeks you’ll notice your heart working more efficiently while you’re smiling.
Light Hiking / Trail Walking
Flat‑trail tips
Choose a well‑maintained, level path—think a city park loop or a flat nature trail. Use a sturdy walking stick for balance, and pause often to catch your breath. Even a 15‑minute stroll on a flat trail counts as low‑impact cardio.
Strength & Flexibility
Resistance Band Circuit
Sample moves
Grab a light‑to‑medium resistance band. Perform 1 set of 10‑12 reps of each, resting 30 seconds between exercises. Repeat 2‑3 times.
- Seated rows – anchor the band at waist height, pull toward you.
- Leg extensions – loop the band around your ankle, straighten the leg.
- Bicep curls – stand on the band, curl upward.
- Side‑leg lifts – band around thighs, lift sideward.
Body‑Weight Moves
Wall push‑ups & seated squats
Wall push‑ups let you control the load while still engaging the chest and shoulders. For seated squats, start from a sturdy chair, stand up using your leg muscles, then sit back down slowly. Both are low‑impact yet effective for older adult fitness.
Yoga & Tai Chi
Gentle flow
A 15‑minute “chair yoga” sequence—slow neck rolls, seated cat‑cow, and easy side bends—improves flexibility and reduces stress hormones. Tai Chi’s slow, dance‑like movements also aid balance, a crucial factor for seniors at risk of falls.
Stretching Routine
Dynamic warm‑up & cool‑down
Begin each session with 5 minutes of dynamic moves: marching in place, arm circles, ankle circles. End with the same muscles relaxed: gentle hamstring stretch, chest opener, and deep breathing for 3‑5 minutes.
Weekly Sample Schedule
| Day | Activity | Duration | Intensity |
|---|---|---|---|
| Monday | Brisk mall walk | 20 min | Moderate (talk test) |
| Tuesday | Resistance band circuit | 15 min | Light |
| Wednesday | Rest & gentle stretching | — | — |
| Thursday | Water aerobics class | 30 min | Moderate |
| Friday | Yoga/Tai Chi | 20 min | Low‑impact |
| Saturday | Recumbent bike + short walk | 25 min | Moderate |
| Sunday | Light hike or leisure walk | 30 min | Easy |
Feel free to swap days to match your calendar, but aim for 3–5 cardio sessions and 2 strength days each week. Consistency is the secret sauce.
Monitoring Progress
Heart‑rate tracking
Use a simple wearable or manually check your pulse every five minutes. For most seniors, staying within 50‑70 % of the age‑predicted maximum (220 – age) is safe. If your heart‑rate feels unusually high, reduce intensity right away.
Symptom log
Keep a tiny notebook or phone note titled “Exercise Log.” Record date, activity, duration, perceived effort, and any symptoms such as chest pressure, dizziness, or excessive breathlessness. Over time the log shows trends and helps your doctor adjust the plan.
Periodic re‑evaluation
Schedule a follow‑up visit (or a repeat stress test) every 6–12 months. Your cardiologist can fine‑tune heart‑rate targets, especially if medication changes.
Hydration & medication timing
Drink water before, during, and after exercise, but avoid large gulps right before a workout if you’re on a diuretic. Also, note that beta‑blockers blunt heart‑rate response, so rely more on the talk test or RPE scale.
Real‑World Success
John, 68, post‑CABG – After his surgeon cleared him, John started with 10‑minute indoor walks, adding two minutes each week. Six months later he can tend his garden for 45 minutes without chest pain, and his doctor reports a 15 % improvement in his stress‑test results.
Martha, 74, living with heart‑failure – Martha incorporated Tai Chi and a resistance‑band routine twice a week. Her six‑minute walk test increased from 300 feet to 460 feet, and she feels more confident climbing stairs at the grocery store.
These stories illustrate how a gradual, heart‑healthy approach can transform daily life. What’s your story? Share it in the comments—you might inspire the next reader!
Common Mistakes
- Skipping warm‑up or cool‑down: Sudden spikes in heart rate can strain the heart.
- Exercising in extreme temperatures: Heat raises heart rate; cold narrows vessels—both increase cardiac load.
- Ignoring medication effects: Beta‑blockers mask pulse rise; you may think you’re over‑exerting when you’re not.
- Choosing high‑impact sports too soon: Running, jumping, or heavy lifting can trigger arrhythmias in fragile hearts.
- Not tracking symptoms: Early warning signs like light‑headedness or chest tightness can be missed without a log.
Conclusion
Regular movement isn’t a luxury for people with heart disease—it’s a proven prescription. By starting slow, choosing low‑impact cardio, adding gentle strength work, and always listening to your body, seniors can protect their hearts, boost stamina, and enjoy everyday activities with far less fear. Follow the sample weekly plan, keep a symptom log, and stay in touch with your cardiologist or cardiac rehab specialist. The safest path to a stronger heart begins with a single step—take it today, and let the benefits build with every mindful movement.
What exercise has worked best for you? Have questions about adapting a routine to your condition? Drop a comment below; we’re all in this together.






















Leave a Reply
You must be logged in to post a comment.