You know those moments when a tiny change feels like a giant leap forward? Like swapping your chunky wired headphones for sleek earbuds—same purpose, but way less hassle, right? Well, imagine that same kind of relief if you’re a heart transplant patient. Turns out, science is finally catching up with convenience. A new blood test could spot organ rejection way earlier than current methods. And get this: no surgical biopsy required. Let’s unpack what this means for you. (Or maybe just your heart’s love story.)
Quick heads-up: If your heart’s recent “upgrade” feels like a whirlwind of checkups, weird diets, and fewer than zero days off, I get it. But here’s the thing: Your transplant team is basically your medical superhero squad. They need to know when that new heart’s throwing a tantrum—aka rejection—before it gets messy. The old way? Repeated heart muscle snatches. The new way? A quick vial of blood. Sounds like a no-brainer, yeah? Let’s dig deeper.
Blood Work, Not Needle Drama
Here’s where the plot thickens. Surgical biopsies? They’ve been the go-to for decades. Your doc sticks a catheter into your heart, yanks out a tiny muscle sample, and checks it for angry immune cells (called cellular rejection). It works… but it’s invasive, uncomfortable, and honestly? Ancient. (Let’s be real—it’s 2025, medicine deserves better Spidey senses.)
Enter the Organ Rejection Biomarker
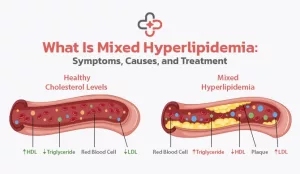
Scientists finally cracked the code: When a heart’s stressed, it sends out little molecular SOS signals (like a bat signal for your blood). The test measures donor DNA fragments—floating like confetti in your bloodstream. Think of it as your new heart whispering, “Hey, the neighborhood’s getting a bit hostile out there…”
Why does this matter? Because sometimes, rejection’s like a slow-burn ember. It smolders without big symptoms until—poof—it’s an inferno. By catching those tiny clues early, we can douse the flames. No more waiting for chest pain or fatigue to scream, “Dude, something’s wrong!”
| Old School Way | New Blood Test |
|---|---|
| Surgical biopsies (monthly the first year) | Simple blood draw (maybe weekly?) |
| Moderate discomfort, risks like bleeding | Virtually no pain or physical risk |
| Diagnosis takes 1-2 days | Results in hours (ultra-fast CRP checks or ctDNA levels) |
| Reactive (after symptoms start) | Potentially preventive (catch rejection before you feel it) |
Your Travel Life After Transplant: Safe or Risky?
So you’re thinking about taking a post-transplant vacation? Join the club. (And yes, I see you, summer-of-2025 bucket listers.) But let’s chat reality: Your immune system’s basically in a fragile salsa-dancing phase after surgery. Travel can be safe… but like dating apps, you gotta pick your destinations carefully.
Best Countries for Heart Transplants & Post-Op Travel
Hearing that Germany or the U.S. are front-runners for heart transplants meant something to my friend Marco. His surgeon in Buenos Aires actually connected him with a Berlin clinic using VR tech to follow up post-op. No doubt, the U.S. leads globally in transplant numbers (nearly 3,700 done in 2020). But Germany? Their long-term heart transplant survival rates are top-shelf stuff. Spain’s not far behind either—great medical infrastructure. (More on that later.)
India? It’s the financial Jedi of medical tourism. Costs can be 60-80% cheaper than the U.S. (Pro tip: Vertical Health tracked a Mumbai clinic with 3D mapping tech that blew some U.S. hubs outta the water.) But—heads-up—the expertise varies city to city. Don’t let a “budget organ” price tag blind you: Rejection needs trustworthy labs for follow-up. Can’t have your dream beach vacation if you’re stuck explaining your new organ to doctors unrelated to your case. (Yeah, that’s from the ISHLT guidelines—Google them, they’re gold.)
Top 5 Post-Transplant Travel “Yes and…” Spots
- USA – Some states prioritize transplant patients, like Texas’s transplant-safe zones near Houston hospitals
- Germany – Got chilly winters? Perfect—plan yours near Heidelberg or Munich clinics with rapid-response blood testing
- Spain – Barcelona or Madrid? Check clinics for blood test availability
- Australia – Melbourne’s St. Vincent Hospital for faster rejection checks post-op
- South Korea – High-tech monitoring + visa-free entries = travel win
But before booking flights, talk to your team. Remember, not all labs can run this new biomarker analysis yet. Oh—and the CDC says steer clear of regions with drought-triggered water contamination (sounds niche, but important—kidneys aren’t fans of tap water surprises, either.)
Even Food Could Be a Double Agent
And here’s where your life gets quirky. Sometimes, when your body upgrades to a new heart (or liver, or lung), it decides someone else’s food allergies are cool now. Imagine going home from your surgery only to discover shellfish—your favorite—is now your nemesis. (Real story from a caregiver on Reddit—I kid you not.)
Ave Maria’s Picture-Perfect Recipe Gone Wrong
A heart transplant patient in Rome, Ave Maria ate her cousin’s rich tomato-shellfish pasta. Two hours later? Hives, swelling, and a frantic ER visit. Turns out her donor family had a huge shellfish allergy lurking in their DNA. Takeaway? Your medical history just adopted tiny pieces of someone else’s quirks. (I mean biologically—we’re not adopting their weird Spotify playlists… unless…)
Why Post-Transplant “Immunosaboteurs” Love Seafood & Nuts
Data from transplant journals consistently finds these suspects appear most regularly as allergens after surgery: eggs, fish, milk, shellfish, and wheat. If your new heart’s buddy had those in their family’s past, you might unknowingly be drawn to dodging them. Think of it as your immune system speed-dating new proteins and deciding, “We’re not compatible.”
Don’t Do This: The Post-Travel Result Nobody Wants
Let’s borrow a cautionary tale. Kyle, 42, felt great post-transplant. Six months later, he booked Machu Picchu without clearing it with his doctor. Enter a bout of fever from contaminated food. By the time he got back, his blood tests showed rejection lurking. Point? Jumping headfirst into travel without checking rejection monitoring options? Not recommended. Especially if your destination’s labs can’t read ctDNA or the latest organ rejection biomarker markers.
Pre-Travel Checklist
- Do destination clinics offer blood tests for transplant monitoring? (See: CareDx adapted global map)
- Have you packed your Sando-K immunosuppressants? (Kapish—don’t lose them.)
- Is your med list in multiple formats? (Digital + paper = clutch.)
- Will avoiding raw charcuterie drive you mad? Probably not worth it, trust me.
You’re not a guinea pig. You’re navigating a new body landscape. That means baby steps first—maybe instead of Peru, start with a cool weekend in Denver or Halifax. Let’s talk risk-adjusted dreams.
Rejection 101: What Your Doctor Won’t Say in 100-Word Paralysis
Organ rejection’s not some rare sci-fi plot twist—it happens to dozens of heart recipients each year. On average, between 15-50% of patients face acute rejection. The ones answering clinic phone calls at 3 a.m. want immediate insight. But invasive biopsies? They’re backlogged, stress-inducing, and let’s be real—they suck. A lot.
Why Blood Tests Should Become Your New Best Friend
The research out of Vanderbilt and UCSD isn’t just pumping out hype. They found that tracking cell-free donor DNA in blood actually spotted rejection weeks earlier than traditional biopsies. Barely a blip on your health radar gets flagged before it becomes catastrophic. That’s like your phone saving you from saying “You’re on mute!” during a Zoom meeting—grace before disaster.
Post-Op Survival Stats: Not Just Rainclouds & Roses
You heard it here first: Numbers aren’t soulless spreadsheets. They tell you if your heart’s got lifespan potential. Let’s cut the fluff:
- Estimated 1-year heart transplant survival in the U.S.: ~85%
- Germany’s 5-year survival after transplant: ~70-76%
- India’s clinics in Mumbai, Chennai? Many match survival stats… but rely more on biopsies than newer blood monitoring
Point? Location matters for care—but so does staying plugged into your rejection tracking. My friend Kalina in Australia? She streams her blood test readings through an app. Her nurse calls every time there’s a user-rejection “wobble.” Yep—tech’s doing outback monitoring now.
Why Travel After Transplant Is Like Dating Post-Breakup: Proceed with Caution
You’re technically in a new long-term medical relationship. Crossing continents to get a test done might not be your best move… initially. Let’s break down why certain places outperform others:
| Country | Rejection Test Readiness | Travel Risk |
|---|---|---|
| United States | Leading-edge ctDNA detection available | Thermopolis, Wyoming not exactly scenic… but biopsies? Bad vibes, best avoided |
| Germany | Bio-sprinting on T-cell analysis & rejection biomarkers | Trusted hospitals in Berlin, Frankfurt, Munich |
| India | Most places still use ELISA-based antibody testing | Lovely destinations—but always confirm your clinic offers newer tests before flight |
| South Korea | Hallyu-wave high-tech cardiac care hospitals | Low-infection-rate hospitals, but language barrier can slow emergency response |
Ever Wonder Why You’re Obsessively Google-Searching “Can Heart Transplant Patients Eat Eggs?”
You should be. Turns out, immunosuppressant drugs can mess with digestion. And some studies (gotta love PubMed) show donor atopic profile can semi-transfer proteins via transplanted organ. Imagine this: You’ve loved scrambled eggs your whole life—then 6 months post-transplant—BOOM—even a single yolk turns your throat itchy. Spooky, right?
Promise & Percentage: Keeping Perspective
Now hold up—this new heart transplant blood test isn’t suddenly replacing everything overnight. Nope. Think of it like GPS replacing paper maps. It’s smarter. Faster. But still… not everywhere. Some hospitals in India and Mexico still do quarterly biopsies. Why? Because funding, access to sequencers, and doctor-comfort zones make it slow to roll out.
Risk caveat time: It’s a great tool but hunts major rejection. Micro stuff? You still need in-person scans sometimes. (Doctors are like chefs—some still like tasting micro fire burns.) Point is: These blood tests help avoid the extreme—the 911 rejections. Vitamin D isn’t a cure. Drugs like cyclosporine are.
Rejection Symptoms: When Your New Heart Starts Voting You Off the Island
So how do you even know if things go sideways? Classic red flags include stuff like:
- Sudden fatigue (like even walking to the door feels intense)
- Palpitations or arrhythmias (your beat’s not your own anymore?)
- Shortness of breath
- Swelling or sudden weight gain
- And—rare but possible—anxiety, nausea, or unexplained sadness
Here’s the kicker: Even trained docs can’t feel rejection through a stethoscope. That’s why tests matter. Because unlike your heart, your blood won’t gaslight you.
The Way Forward (And Why Donors Sometimes Haunt You in Food) — literally?
Look, your heart didn’t come with an owner’s manual, yeah? But as we learn more…
- Biomarkers (like ctDNA screening) could become standard post-op protocols
- Meal choices matter more—if you suddenly hate peanut butter, maybe Dr. Google is onto something
- Travel could become safer—but your immunosuppressants may demand tighter hotel sanitization
You’ll hop onto video calls with investigators in Miami, meet researchers tracking transplant durability, even find support groups where people have cooler comeback stories than your Netflix binging saga. The key? Don’t just wing it—plan, prep, and punch the fear factor right in the face.
So… if this sounds like a winning combo, hit reply with your dream destination—or a weird food scare you encountered. I wanna hear it. We’re writing this chapter together.
Final Thought:
Life after a heart transplant is like utterly rewriting your personal history notebook. Just when you think you’ve got it—or your route planned—n ew tests, allergens, and travel realities overwrite old rules. Let’s appreciate the wins: losing blades, gaining time. (And yes, even overhauling your Parmesan sprinkler habits.)
If this feels like the info you’ve been longing for post-op, don’t keep it to yourself. Let’s help each other navigate—and maybe add a “new heart-friendly recipe” folder and map at the same time. Stay sharp, stay curious. This is your roadmap now—no GPS monotone, but passion, experience, and a few travel regrets to laugh about eventually.






















Leave a Reply
You must be logged in to post a comment.