Quick Answer
In a nutshell, mixed hyperlipidemia is the condition where both cholesterol and triglycerides are elevated, and the correct ICD‑10‑CM code to capture it is E78.2. This code is billable, effective from 1 Oct 2024 (the 2025 edition), and it lets your provider document the disorder accurately for both clinical care and reimbursement.
Need a quick refresher on what mixed hyperlipidemia actually means? Check out mixed hyperlipidemia meaning for a plain‑language overview.
What Is Mixed Hyperlipidemia
Definition & Pathophysiology
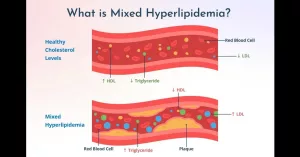
Mixed hyperlipidemia is a type of lipid disorder in which a person’s blood shows high levels of low‑density lipoprotein (LDL) cholesterol and triglycerides at the same time. Think of it as a “double‑whammy” for your arteries: the LDL builds up plaque while the triglycerides make the blood more viscous, both raising cardiovascular risk.
The condition often runs in families. Classic genetic forms‑—the Fredrickson type IIb and type III patterns—are linked to mutations in the apolipoprotein B‑100 gene or other genes that affect how the body clears lipoproteins. In everyday practice, though, many patients develop mixed hyperlipidemia because of lifestyle factors (poor diet, sedentary habits), obesity, diabetes, or metabolic syndrome.
How It Differs From Pure Forms
| Feature | Mixed Hyperlipidemia (E78.2) | Pure Hypercholesterolemia (E78.0) | Pure Hypertriglyceridemia (E78.1) |
|---|---|---|---|
| Key labs | Elevated LDL + high TG | High LDL only | High TG only |
| Common causes | Family history + diet + diabetes | Genetic (LDL‑R mutation) | Alcohol, uncontrolled diabetes |
| Cardiovascular risk | 2‑3× higher than single‑lipid rise | Elevated but lower than mixed | Elevated, especially if TG > 500 mg/dL |
Related Terminology
If you’re still wondering “what is mixed hyperlipidemia?” the answer is simple: it’s a lipid profile that shows both cholesterol and triglyceride excess. See also What is mixed hyperlipidemia for a deeper dive.
ICD‑10 Code E78.2 Details
Official Description
According to the ICD‑10‑Data entry for E78.2, the code is defined as “Mixed hyperlipidemia.” It is a billable/specific diagnosis that became effective on 1 Oct 2024 for the 2025 fiscal year. The code is used when a patient presents with a combination of elevated cholesterol and triglycerides that cannot be explained solely by a pure hyperlipidemia classification.
Applicable To (What E78.2 Covers)
| Applicable Conditions |
|---|
| Broad‑ or floating‑betalipoproteinemia |
| Combined hyperlipidemia NOS |
| Elevated cholesterol with elevated triglycerides NEC |
| Fredrickson’s hyperlipoproteinemia, type IIb or III |
| Hyperbetalipoproteinemia with pre‑betalipoproteinemia |
| Hypercholesteremia with endogenous hyperglyceridemia |
| Hyperlipidemia, group C |
| Tubo‑eruptive xanthoma |
| Xanthoma tuberosum |
Exclusions (When Not to Use E78.2)
There are two “Type 1 excludes” that should never accompany E78.2:
- Cerebrotendinous cholesterosis (E75.5)
- Familial combined hyperlipidemia (E78.49)
If the patient’s condition fits one of those excluded diagnoses, you’d pick the appropriate separate code instead.
Documenting in the EMR
When you or your clinician writes the note, a clean way to capture the diagnosis is:
Patient presents with mixed hyperlipidemia, ICD‑10 E78.2.
Adding a brief rationale—e.g., “LDL = 165 mg/dL, TG = 280 mg/dL” —helps coders avoid “upcoding” errors and ensures the claim is accepted.
Clinical Implications & Treatment
Why Accurate Coding Matters
Beyond the paperwork, the right code triggers the right care pathways. Insurance companies often tie coverage of lipid‑lowering meds, dietary counseling, and repeat labs to a documented diagnosis of mixed hyperlipidemia. Moreover, quality‑measure programs (like HEDIS) look for E78.2 to gauge how well a practice manages high‑risk patients.
Standard Treatment Options
Mixed hyperlipidemia usually calls for a two‑pronged approach: lifestyle changes and medication.
- Diet & Exercise: Reduce saturated fats, limit sugary drinks, aim for 150 minutes of moderate activity weekly. Even modest weight loss (5‑10 % of body weight) can drop triglycerides by 20‑30 %.
- Statins: First‑line for lowering LDL; they also modestly lower triglycerides.
- Fibrates or Omega‑3 EPA/DHA: Target high triglycerides directly.
- PCSK9 inhibitors: For patients who can’t reach goals with statins alone.
Guidelines from the 2024 ACC/AHA Lipid Management Consensus suggest a stepwise escalation: start with a statin, add a fibrate or high‑dose omega‑3 if TG remains >200 mg/dL, and consider PCSK9 inhibitors for very high‑risk patients.
Impact on Life Expectancy & Cardiovascular Risk
Studies show that patients with both elevated LDL and triglycerides face roughly a 2‑3‑fold increase in atherosclerotic cardiovascular disease (ASCVD) events compared to those with a single‑lipid abnormality. However, with proper treatment, risk can be halved or even reduced to near‑baseline levels. For a hopeful outlook, see mixed hyperlipidemia life expectancy—the data is encouraging when therapy is adhered to.
Billing & Reimbursement Tips
When E78.2 Is Billable
The 2025 fiscal year (Oct 1 2024 – Sept 30 2025) recognizes E78.2 as a valid, reimbursable diagnosis for HIPAA‑covered transactions. Pair it with the appropriate CPT code for the lab work—most commonly 80061 (Lipid panel) or 82465 (Total cholesterol). Here’s a sample claim line:
CPT 80061 – Lipid Panel Diagnosis: E78.2
Common Coding Pitfalls
- Choosing E78.0 or E78.1 when both LDL and TG are high (that’s a mis‑code).
- Omitting the “NEC” (Not Elsewhere Classified) note when the pattern doesn’t fit a specific subtype.
- Using E78.49 (familial combined hyperlipidemia) when the exclusion criteria apply.
To avoid these hiccups, run a quick audit: pull all claims with E78.2, verify the lab values, and flag any that only show a single‑lipid elevation.
Auditing Checklist for Coders
- Confirm LDL > 130 mg/dL AND TG > 150 mg/dL.
- Check for any exclusion codes (E75.5, E78.49).
- Ensure the encounter includes a lipid panel CPT.
- Document the rationale in the clinical note.
- Validate that the payer’s policy accepts E78.2 for the service date.
Conclusion
Understanding that mixed hyperlipidemia is coded as E78.2 is more than a bureaucratic detail—it’s the gateway to better care, clearer communication, and smarter billing. By recognizing the condition’s dual‑lipid nature, you can work with your provider to choose the right lifestyle tweaks and medications, lowering both your cholesterol and triglyceride numbers, and ultimately protecting your heart.
Remember, accurate coding not only keeps the insurance paperwork moving but also flags you for the latest guideline‑driven therapies. If you’ve ever felt lost in the sea of medical codes, I hope this friendly walk‑through makes the journey feel a little less intimidating.
Got questions about how to talk to your doctor about E78.2, or want to share your own success story with mixed hyperlipidemia treatment? Feel free to reach out—your experience could help someone else navigate the same road.
























Leave a Reply
You must be logged in to post a comment.