Disorders such as myasthenia gravis, multiple sclerosis, and various motor neuron conditions can resemble amyotrophic lateral sclerosis (ALS) because they produce similar signs. Physicians often rely on multiple investigations to exclude alternative diagnoses.
ALS is a degenerative neurological disease marked by the gradual loss of motor neurons in the brain and spinal cord, resulting in progressive muscle weakness and wasting.
Yet several illnesses imitate ALS due to symptom overlap, complicating an accurate diagnosis. It can take more than a year to reach a definitive ALS diagnosis in some cases.
Continue reading to learn about conditions that can be confused with ALS and how clinicians distinguish them from true ALS.
Symptoms of ALS
Typical ALS symptoms include:
- muscle weakness
- muscle wasting
- fasciculations (twitching)
- muscle stiffness
- trouble swallowing (dysphagia)
- speech difficulties (dysarthria)
- breathing impairment
- fatigue
Myasthenia gravis
Myasthenia gravis (MG) is a neuromuscular autoimmune disorder that can be mistaken for ALS because both cause weakness. However, there are notable distinctions.
MG commonly causes fluctuating weakness that worsens with activity and often begins in the eye muscles, as described here.
Clinicians separate MG from ALS using specialized studies such as repetitive nerve stimulation, which demonstrates a typical decremental response. Blood tests can also detect antibodies to the acetylcholine receptor or muscle-specific kinase, supporting an MG diagnosis.
Unlike ALS, a relentlessly progressive disease with no cure, MG has effective therapies including acetylcholinesterase inhibitors and immunosuppressive drugs.
Multiple sclerosis
Multiple sclerosis (MS) is another neurological disorder that sometimes resembles ALS because of shared features. MS more commonly presents with episodic neurological deficits that remit and relapse, whereas ALS shows continual, progressive degeneration of motor neurons.
Imaging with MRI can reveal the characteristic lesions of MS in the central nervous system, aiding differentiation. Cerebrospinal fluid analysis may also help distinguish MS from ALS.
Unlike ALS, MS has disease-modifying therapies that can manage symptoms and slow disease progression.
Other motor neuron disorders
Several motor neuron syndromes can look like ALS, including:
- Primary lateral sclerosis (PLS): PLS is an uncommon motor neuron disease marked by progressive weakness, stiffness, and spasticity in the limbs. Unlike ALS, PLS predominantly affects upper motor neurons.
- Progressive muscular atrophy (PMA): PMA primarily involves lower motor neurons, causing muscle weakness and wasting. It resembles ALS but lacks the upper motor neuron signs often seen in ALS.
- Hereditary spastic paraplegia (HSP): This group of inherited disorders causes spasticity and weakness, frequently beginning in the legs. While it shares spasticity with ALS, it doesn’t entail the same motor neuron degeneration.
- Kennedy’s disease: This rare genetic condition mainly affects the bulbar and spinal regions, producing weakness and muscle loss. It can mimic ALS but is distinguishable through genetic testing; it is X-linked and predominantly affects males.
Key terms
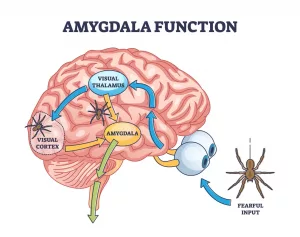
Motor neuron degeneration impairs the nerve signals that control muscles. Nerve cells fail to transmit commands from the brain and spinal cord to muscles, causing muscle wasting. As it advances, it may impact functions such as speaking or swallowing.
Spasticity refers to muscle tightness or increased tone and can lead to uncontrolled movements; it is a feature of several motor neuron disorders.
Upper motor neurons originate in the cerebral cortex and descend to the spinal cord. Lower motor neurons arise in the spinal cord and extend to muscles.
Infections
Infectious diseases like Lyme disease and HIV can produce neurological symptoms that imitate ALS.
Lyme disease may cause neurological manifestations such as weakness and spasticity. Differentiation from ALS relies on a careful history and blood testing for Lyme antibodies.
Neurological complications related to HIV, including motor dysfunction, can also resemble ALS. Distinction depends on HIV testing and assessment of other HIV-associated signs.
Hyperthyroidism
Hyperthyroidism can mimic ALS because it may cause muscle weakness, tremor, and weight loss. Thyroid function tests reveal elevated thyroid hormones to differentiate it from ALS.
Treatment of hyperthyroidism with antithyroid medications or radioactive iodine can resolve these symptoms.
Vitamin B12 deficiency
Deficiency of vitamin B12 can produce neurological symptoms similar to ALS, such as weakness and sensory changes. Blood testing that demonstrates low B12 levels confirms the deficiency.
B12 supplementation can reverse these manifestations, distinguishing it from the irreversible course of ALS.
Post-polio syndrome
Post-polio syndrome may present with muscle weakness and fatigue that can be confused with ALS. A prior history of poliomyelitis and electromyography (EMG) findings help separate it from ALS.
Unlike ALS, weakness in post-polio syndrome tends to be more stable, and management focuses on rehabilitation to maximize function.
Nerve damage
Spinal cord compression (myelopathy) or a compressed nerve root (radiculopathy), especially in the neck or lower back, can produce symptoms resembling ALS and may show overlapping findings on tests like EMG.
In addition to motor deficits, radiculopathy commonly causes sensory loss and neuropathic pain—features not usually seen in ALS. Also, unlike ALS, myelopathy may cause severe neck pain and sphincter dysfunction.
How do doctors confirm or exclude ALS?
Clinicians combine a thorough clinical assessment of symptoms and history with diagnostic tests to either confirm or exclude ALS, including:
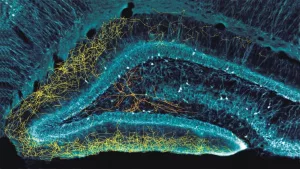
- EMG and nerve conduction studies: These evaluate electrical activity in muscles and peripheral nerves. In ALS, EMG often shows signs of denervation and spontaneous muscle activity.
- MRI and CT scans: Imaging helps rule out other disorders that can mimic ALS. While not diagnostic for ALS, they may show muscle wasting or structural abnormalities.
- Blood tests: Laboratory testing is used to exclude other causes of similar symptoms, such as thyroid disease or infections. ALS does not have a specific blood biomarker.
- Genetic testing: For familial cases, genetic testing can identify known ALS-related mutations when indicated.
Frequently asked questions
Below are common questions about conditions that mimic ALS.
How often is ALS misdiagnosed?
ALS is initially misdiagnosed in roughly 10% of patients, often because other conditions can present similarly.
How long does it take to diagnose ALS?
Diagnosis can take several months; on average it ranges from 10 to 16 months from symptom onset to confirmation.
What is the tongue test for ALS?
There is no formal “tongue test” for ALS. Clinicians assess tongue strength as part of the neurological exam to evaluate motor neuron function.
Tongue fasciculations (twitching) can be an early feature of ALS, but they are not specific to ALS alone.
Takeaway
Many disorders produce symptoms similar to ALS, such as weakness, twitching, and muscle wasting. Frequent mimics include MG, MS, and other motor neuron conditions. For comparisons of skin-related mimics, see shingles vs eczema and shingles vs poison ivy.
Physicians use a combination of clinical assessment, targeted tests, and exclusion criteria to tell ALS apart from conditions that mimic it. Seeking medical attention early for concerning symptoms can help begin the often lengthy diagnostic process sooner.






















Leave a Reply
You must be logged in to post a comment.