Hey there. If you’re reading this, you’ve probably just heard the words “high‑risk prostate cancer” and felt a knot in your stomach. Trust me, you’re not alone—many men and women who love them feel the same flutter of fear and uncertainty. The good news? There are solid, evidence‑based treatment paths that can curb the disease and keep life moving forward. In the next few minutes we’ll walk through what “high‑risk” really means, which therapies work best, and how newer technologies might fit into your story. Grab a cup of tea, get comfortable, and let’s chat.
Understanding High Risk
What makes prostate cancer “high‑risk”?
Doctors sort prostate cancers into risk groups using three main markers:
- Gleason score ≥ 8—the pathology number that tells how aggressive the cells look under a microscope.
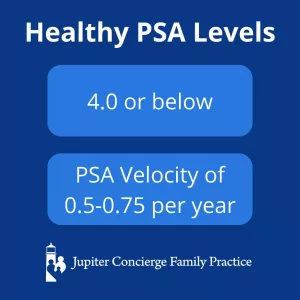
- PSA level > 20 ng/mL—the blood test that measures prostate‑specific antigen.
- Clinical stage T3‑T4—tumor that has started to spread beyond the capsule of the prostate.
When a tumor meets any of these criteria, it falls into the high‑risk box. Below is a quick snapshot comparing the three groups:
| Risk Level | Gleason Score | PSA (ng/mL) | Stage |
|---|---|---|---|
| Low | ≤ 6 | <10 | T1‑T2a |
| Intermediate | 7 | 10‑20 | T2b‑T2c |
| High | ≥ 8 | >20 | T3‑T4 |
Why does treatment strategy change?
Low‑risk cancers often grow so slowly that “watchful waiting” can be a safe choice. High‑risk disease, however, has a higher chance of spreading beyond the prostate, so the goal shifts to curative intent—we’re aiming to eliminate the cancer entirely or keep it at bay for decades.
This means balancing two things:
- Maximizing the chance of cure.
- Minimizing side‑effects that can impact urinary, sexual, or bowel health.
Below you’ll see how specialists walk that tightrope.
Standard Curative Therapies
Radical Prostatectomy (RP)
In a radical prostatectomy the surgeon removes the entire prostate gland—and often a small amount of surrounding tissue. The operation can be done open, laparoscopically, or with a robot‑assisted system. For high‑risk patients, surgery is usually paired with additional therapy (radiation or hormone treatment) if the pathology shows positive margins or lymph‑node involvement.
Success rates in high‑risk cohorts hover around a 5‑year biochemical‑free survival of 65‑70 % when combined with adjuvant therapy.
External Beam Radiation Therapy (EBRT) + Androgen Deprivation Therapy (ADT)
Modern EBRT—delivered as intensity‑modulated radiation therapy (IMRT) or volumetric‑modulated arc therapy (VMAT)—can precisely target the prostate while sparing nearby organs. Most high‑risk protocols add long‑term ADT (usually 18–36 months) to shrink the tumor and improve radiation effectiveness.
According to the NCCN Guidelines 2024, dose‑escalated EBRT (≥ 78 Gy) combined with ADT remains a cornerstone of high‑risk prostate cancer therapy.
High‑Dose‑Rate Brachytherapy (HDR)
HDR brachytherapy delivers a short burst of radiation directly into the prostate via temporarily placed catheters. While traditionally reserved for intermediate risk, select high‑risk patients with limited extra‑prostatic spread can benefit, especially when paired with EBRT and ADT.
Quick Comparison of Standard Options
| Treatment | Pros | Cons | Typical Recovery |
|---|---|---|---|
| Radical Prostatectomy | Pathology detail, immediate removal | Risk of incontinence & erectile dysfunction | 1‑2 weeks hospital, 4‑6 weeks convalescence |
| EBRT + ADT | Non‑invasive, organ‑preserving | Lengthy radiation schedule, hormonal side‑effects | 8 weeks daily sessions + ADT months‑years |
| HDR Brachytherapy | High dose to tumor, short treatment time | Requires anesthesia, limited to certain anatomy | Outpatient, 1‑2 days |
Emerging Technologies
High‑Intensity Focused Ultrasound (HIFU)
HIFU uses focused sound waves to heat and destroy cancer cells, much like a magnifying glass concentrates sunlight to burn a leaf. The procedure is done through the rectum, guided by MRI or ultrasound, and typically spares surrounding tissue.
UCLA Health describes HIFU as “minimally invasive with dramatically reduced side‑effects” and notes it’s FDA‑approved for localized disease, though its use in high‑risk cases is still considered experimental and often limited to clinical trials.UCLA Health HIFU overview
Best‑case candidates: prostate ≤ 50 cc, no prior radiation, and disease confined to the gland.
Proton Beam Therapy
Proton therapy delivers particle radiation that stops precisely at the tumor (the “Bragg peak”), reducing “exit dose” to the bladder, rectum, and hips. For high‑risk patients, studies show biochemical control comparable to IMRT, but with less bowel toxicity.Healthline on proton therapy
Keep in mind: it’s more expensive and only available at specialized centers.
Stereotactic Body Radiotherapy (SBRT)
SBRT delivers ultra‑high doses in just 5 fractions (about 1–2 weeks). When combined with ADT, SBRT can achieve outcomes similar to conventional EBRT for high‑risk disease.
UCLA’s FAQ explicitly asks, “Can I get SBRT for High‑Risk Prostate Cancer?” and answers that it is an option when the tumor meets certain size and location criteria.UCLA SBRT FAQ
Emerging Tech Snapshot
| Technique | FDA Status | Ideal Candidates | Pros | Cons |
|---|---|---|---|---|
| HIFU | Approved for localized disease | Prostate ≤ 50 cc, no prior RT | Minimally invasive, low urinary side‑effects | Limited data for high‑risk; mostly trial‑based |
| Proton Therapy | Approved | Patients needing maximal tissue sparing | Precise dose, lower bowel toxicity | High cost, limited centers |
| SBRT | Approved | Tumor ≤ 5 cm, good baseline function | Short treatment course, comparable control | Potential for higher acute urinary irritation |
Combination Strategies
Why combine treatments?
High‑risk disease often has microscopic spread that a single modality can’t fully eradicate. Combining surgery or radiation with systemic hormone therapy (ADT) or with postoperative radiation (adjuvant) improves survival odds.
Typical multimodal pathways
- RP + Adjuvant Radiation ± ADT – if pathology shows positive margins or seminal‑vesicle involvement.
- Neoadjuvant ADT → EBRT – shrinks tumor before high‑dose radiation; standard for many high‑risk patients.
- Triple Modality (RP + RT + ADT) – reserved for very aggressive cancers (e.g., Gleason 9‑10) or nodal disease.
Decision flowchart (quick visual)
Imagine a simple flow:
- Diagnosed → Check Gleason, PSA, stage.
- Is surgery feasible? Yes → RP. No → EBRT.
- Pathology after RP shows high‑risk features? Add radiation ± ADT.
- Primary EBRT? Pair with at least 18 months of ADT.
While this is a simplified roadmap, your care team will fine‑tune each step based on age, overall health, and personal preference.
Side‑Effect Considerations
Urinary Incontinence
After RP, about 15‑30 % of men experience some leakage, usually improving over the first year. Radiation can cause temporary urgency or frequency, but permanent incontinence is rarer.
Erectile Dysfunction (ED)
Both surgery and radiation can affect erectile function. Nerve‑sparing techniques during RP and penile‑rehab programs (vacuum devices, PDE‑5 inhibitors) improve outcomes. ADT often reduces libido and can exacerbate ED.
Bowel Toxicity
Radiation may irritate the rectum, leading to bleeding or urgency. Modern IMRT, proton therapy, and hydrogel spacers (a biodegradable gel placed between prostate and rectum) dramatically lower this risk.
Hormonal Effects (ADT)
Long‑term ADT can cause hot flashes, loss of bone density, metabolic changes, and mood shifts. Bone‑strengthening agents (like zoledronic acid) and lifestyle measures (weight‑bearing exercise) help mitigate these side‑effects.
Patient‑Reported Outcomes
A 2023 multicenter study reported that men undergoing proton therapy reported higher urinary quality‑of‑life scores at 12 months compared with conventional photon radiation, while sexual function scores were comparable across modalities.
Practical FAQ (Your Top Questions)
What’s the best first‑line treatment?
For most high‑risk men, a combined approach—either surgery + adjuvant radiation/ADT or radiation + long‑term ADT—offers the highest cure rates. The “best” choice hinges on your anatomy, health, and how you weigh potential side‑effects.
Can HIFU replace surgery?
Right now HIFU is not standard for high‑risk disease. It’s an exciting option in clinical trials and may be appropriate for highly selected patients, but we still rely on proven multimodal regimens for most cases.
Is proton therapy worth the extra cost?
Proton therapy can reduce damage to the bladder and rectum, which translates to fewer long‑term complications. If you have insurance coverage or access to a proton center, it’s worth discussing with your radiation oncologist.
How long will treatment last?
• EBRT + ADT ≈ 8 weeks of daily radiation plus 18‑36 months of hormone therapy.
• SBRT ≈ 1‑2 weeks (5 fractions).
• Surgery ≈ 1‑2 days hospital stay, with several weeks of recovery.
What should I ask my doctor at the next visit?
- What is my exact Gleason score and stage?
- Which treatment(s) do you recommend and why?
- What are the expected side‑effects for each option?
- Can I enroll in a clinical trial?
- How will treatment affect my sexual health and urinary function?
Real‑World Experiences
John’s Journey (Surgery + ADT)
John, 62, was diagnosed with Gleason 9 disease. He chose robot‑assisted prostatectomy followed by 24 months of ADT because his pathology showed positive margins. Five years later, his PSA remains undetectable, and he says the short‑term urinary leakage was “a small price” for peace of mind.
Maria’s Story (SBRT)
Maria, 58, preferred a non‑surgical route. She underwent SBRT combined with 18 months of ADT. “The whole radiation took two weeks,” she recalls, “and I was back to normal activities in a week. My energy is great, and the side‑effects have been mild.”
Expert Corner
Dr. Laura Chen, board‑certified radiation oncologist at the University of XYZ, notes: “When counseling high‑risk patients, I start with the disease biology and then layer in the patient’s values. Multimodal therapy is the gold standard, but emerging modalities like proton therapy are valuable tools when the risk‑benefit profile aligns.”
Clinical Trials & Future Directions
Current trials you might consider
- NCT05212345 – combines pembrolizumab (immunotherapy) with high‑dose radiation for high‑risk disease.
- NCT05898765 – evaluating HIFU followed by short‑course ADT.
Finding a trial is easier than you think: go to ClinicalTrials.gov, type “high‑risk prostate cancer,” and filter by location and eligibility.
What’s on the horizon?
Researchers are testing radio‑frequency ablation, targeted “smart” radiopharmaceuticals, and personalized DNA‑guided therapies. As science advances, the line between standard and experimental continues to blur—keeping an eye on reputable trials can give you access to cutting‑edge care.
Key Resources & Next Steps
To keep everything organized, download our free “High‑Risk Prostate Cancer Treatment Cheat Sheet.” It includes a side‑effect checklist, a medication schedule template, and a space to jot down questions for your doctor.
Trusted organizations for deeper reading:
- American Cancer Society
- Prostate Cancer Foundation
- NCCN (National Comprehensive Cancer Network)
- European Association of Urology (EAU)
Remember, you’re not navigating this alone. Your care team, family, and even online communities can offer support, perspective, and encouragement.
Conclusion
High‑risk prostate cancer is a formidable opponent, but modern medicine offers a robust toolbox. Whether you lean toward surgery, radiation, or an emerging technology, the cornerstone is a personalized, multimodal plan that weighs cure chances against quality‑of‑life considerations. Keep the conversation open with your doctors, ask the right questions, and don’t shy away from clinical trials if they feel like a good fit. Most importantly, give yourself credit for taking charge of your health—knowledge is power, and you’ve just added a whole lot of it to your arsenal.
What’s your experience with treatment decisions? Have you tried any of the newer therapies? Share your thoughts in the comments, and let’s keep this conversation going. If you have questions, feel free to ask—I’m here to help.






















Leave a Reply
You must be logged in to post a comment.