Medicare provides coverage for one annual prostate-specific antigen (PSA) screening for individuals with prostates, provided they satisfy the eligibility requirements and the screening is considered medically necessary.
Typically, Medicare Part B (medical insurance) or Medicare Part C (Medicare Advantage) will cover one PSA blood test per year. You must, however, meet the program’s eligibility standards and receive the test from a clinician who accepts Medicare assignment or is in-network for your Advantage plan.
The PSA test is a simple blood draw that measures the level of prostate-specific antigen in the bloodstream. Elevated PSA readings can signal the presence of prostate adenocarcinoma before symptoms appear, though increased PSA can also result from benign conditions that raise PSA levels.
Continue reading to understand the eligibility rules for annual PSA testing under Medicare, expected costs, and what additional services Medicare might cover.
Who qualifies for PSA screening under Medicare?
Medicare covers preventive services including one yearly PSA blood test for people with prostates if they satisfy the following conditions:
- are older than 50 years
- at least 11 months have elapsed since your prior PSA test
- the screening is ordered by your healthcare provider and is deemed medically necessary
Medicare also covers an annual preventive digital rectal exam.
What will the PSA test cost with Medicare?
If your healthcare provider “accepts assignment,” the PSA blood test will be covered with no charge under Medicare.
You might incur extra fees for the clinician’s services if the provider does not accept assignment.
For those enrolled in Medicare Part C (Medicare Advantage), your plan should at a minimum match Original Medicare (Parts A and B) coverage. Nonetheless, to limit out-of-pocket spending, you may need to confirm that your provider is in-network for your specific Advantage plan.
What happens if the PSA test is elevated—what does Medicare cover?
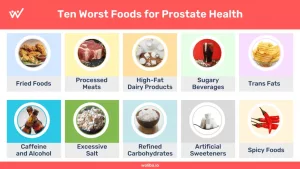
An elevated PSA can indicate prostate cancer, but higher PSA levels may also be due to noncancerous causes, such as:
- benign prostatic hyperplasia (BPH), or an enlarged prostate
- prostatitis, meaning an inflamed prostate
- urinary tract infection (UTI)
- recent sexual activity or ejaculation
If your PSA result is high, further evaluation may be necessary to clarify the cause. This could include repeat blood tests or imaging studies. If cancer is suspected, a clinician may advise a prostate biopsy to look for malignant cells.
Medicare covers these diagnostic procedures and also covers FDA-approved treatments for prostate cancer.
Common questions
Why might Medicare deny coverage for my PSA test?
Medicare may deny payment if your clinician did not order the PSA test or did not document it as medically necessary. Denials can also occur if the test is done before at least 11 months have passed since your previous PSA screening.
How much does a PSA blood test typically cost?
When you meet Medicare’s conditions, a PSA blood test is generally free. Without insurance, PSA testing costs vary widely—often under $100 to $300 or more—depending on whether you use an at-home kit or go to a clinic or lab.
How frequently should a 65-year-old get a PSA test?
The American Cancer Society suggests annual PSA screening for people with prostates whose PSA is 2.5 ng/mL or higher. Those with PSA levels below that threshold may be screened every two years instead.
What is a free PSA test and is it covered by Medicare?
Clinicians may order a free PSA test if initial PSA results are elevated. A free PSA test measures the portion of PSA in the blood that is unbound to proteins.
Free PSA is not categorized as a Medicare preventive service. You could be responsible for your Medicare Part B premium and for paying roughly 20% of approved charges for Medicare-covered services after meeting any deductible.
Bottom line
Medicare covers one annual PSA screening and one digital rectal exam to facilitate early detection of prostate cancer. These preventive checks can help identify prostate cancer before symptoms arise and typically prior to cancer spread, which can lead to better treatment outcomes.
To receive full coverage, a clinician must determine the test is medically necessary and you must meet Medicare’s eligibility criteria. The provider must also accept the Medicare-approved payment amount.
If you carry a Medicare Advantage policy, you may need to see an in-network clinician or attend an in-network facility for the screening to be covered by your plan.
Related resources: does medicare cover paxlovid; does medicare cover holter monitor; does medicare cover cortisone shots




















Leave a Reply
You must be logged in to post a comment.