If you’ve landed on this page, chances are you (or someone you love) are wondering how bulimia is actually treated. The short answer? A blend of talk therapy, medication, and nutrition counseling—tailored to the person’s needs, goals, and life circumstances. It might sound like a lot, but each piece fits together like a puzzle, helping you move from a cycle of binge‑purge to a healthier, steadier rhythm.
Below you’ll find a friendly, step‑by‑step guide that explains why a multi‑component approach works, the different therapy styles you’ll hear about, the medicines that can help, and the nutrition strategies that support real recovery. I’ve woven in research from respected sources (NHS, Mayo Clinic, Beat) and personal‑style anecdotes so you feel both informed and encouraged.
Why Multi-Component Works
What “bulimia treatment” really means
Bulimia nervosa is more than just “eating too much and then vomiting.” It’s a complex mental‑health condition where thoughts, emotions, and body signals get tangled together. When we talk about bulimia treatment, we’re really talking about a coordinated plan that tackles the psychological urge to binge, the physical impacts of purging, and the underlying nutritional imbalances.
How therapy, medication, and nutrition fit together
Think of each component as a teammate on a relay‑race team. Therapy helps you develop healthier thinking patterns, medication can calm the brain chemistry that fuels urges, and nutrition restores your body’s fuel tank. When one teammate falters, the others can still keep you moving forward—but the best results happen when they pass the baton smoothly.
Core Components Comparison
| Component | Primary Goal | Typical Duration | Example Tools |
|---|---|---|---|
| Therapy (CBT‑E, FBT, DBT…) | Change thoughts & behaviors that drive binge‑purge cycles | 16‑20 weeks (often ongoing support) | Worksheets, exposure exercises, mindfulness drills |
| Medication (Fluoxetine, other SSRIs) | Reduce urges, treat co‑occurring anxiety/depression | 6‑12 months, then evaluation | Daily pill regimen, regular blood‑test monitoring |
| Nutrition counseling | Stabilize eating patterns, replenish nutrients | Ongoing, often weekly at start | Meal plans, food‑frequency logs, appetite‑rating scales |
Therapy Options
Cognitive Behavioral Therapy (CBT‑E)
CBT‑E (Enhanced Cognitive Behavioral Therapy) is the gold‑standard for bulimia. It teaches you to spot the “thought‑eating‑behavior” loop, challenge the distorted beliefs (“I’m a failure if I eat a cookie”) and replace the binge‑purge response with healthier coping skills. Studies from Mayo Clinic show remission rates of up to 60 % when CBT‑E is combined with medication.
Family‑Based Therapy (FBT)
For teens, FBT brings parents into the treatment room as allies, not critics. The family learns how to structure meals, monitor behaviors, and provide a supportive environment. According to the UK’s NICE guidelines, FBT often outperforms individual therapy for younger patients because it tackles the home dynamics that can trigger binge‑purge cycles.
Dialectical Behavior Therapy (DBT)
DBT shines when emotional dysregulation is a big driver of binge episodes. It offers four skill sets—mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. Imagine DBT as a toolbox that helps you stay calm when anxiety knocks at the door, so you don’t “run to the fridge” for comfort.
Other Evidence‑Based Modalities
- Acceptance & Commitment Therapy (ACT) – teaches you to observe thoughts without fighting them.
- Interpersonal Therapy (IPT) – focuses on relationship issues that may fuel disordered eating.
- Schema Therapy – digs deep into long‑standing belief patterns.
Choosing the Right Modality
Here’s a quick decision‑tree you can run in your mind:
- Are you under 18? → FBT or CBT‑E.
- Is anxiety or mood swings your main trigger? → DBT or ACT.
- Do you prefer a structured, step‑by‑step plan? → CBT‑E.
- Do you want the whole family involved? → FBT.
Real‑World Example
Emily (22) started with CBT‑E and felt the urges lessen, but after a stressful job change she slipped back into bingeing. Her therapist suggested adding DBT skills for distress tolerance. Within a month, Emily reported feeling “more in control of my emotions, not just my eating.” Stories like Emily’s illustrate why many clinicians blend approaches to fit the evolving needs of each person.
Medication Choices
Fluoxetine: The FDA‑Approved Option
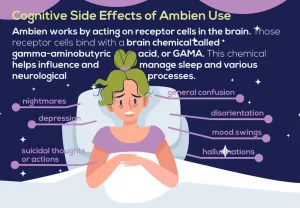
Fluoxetine (Prozac) is the only medication officially approved by the FDA for bulimia. It’s an SSRI that can dampen binge urges and improve mood. Typical dosing starts at 20 mg daily and may rise to 60 mg. Side effects can include nausea, sleep changes, or mild headache—most of which fade after a few weeks.
Off‑Label Antidepressants
When fluoxetine isn’t tolerated, clinicians sometimes try other SSRIs like sertraline (Zoloft) or citalopram. These aren’t officially approved for bulimia but help with the same serotonin pathways. According to WebMD, these off‑label options can be effective, especially when anxiety co‑exists.
Combining Meds with Therapy
The strongest evidence shows that medication works best when paired with therapy—think of meds as the “engine starter” and therapy as the “road map.” A NHS review notes that combined treatment raises remission odds by 30 % compared with therapy alone.
Risks & Monitoring
Because many people with bulimia also experience electrolyte disturbances from vomiting, it’s crucial to avoid medications that raise seizure risk, such as bupropion (Wellbutrin). Regular blood tests, weight checks, and open communication with your prescriber keep you safe.
Medication Appointment Checklist
- Ask: “Will this medication affect my appetite or weight?”
- Ask: “What side‑effects should I watch for?”
- Ask: “How long before I should notice a benefit?”
- Bring a list of current supplements or over‑the‑counter meds.
Nutrition & Lifestyle Support
Why a Dietitian Matters
Purging can strip the body of essential electrolytes, vitamins, and minerals. A registered dietitian who specializes in eating disorders designs a balanced meal plan, monitors lab results, and helps you rebuild a healthy relationship with food. According to the NHS, nutrition counseling is a core pillar of bulimia treatment.
Core Nutrition Strategies
1. Regular meals and snacks – aim for three meals plus two snacks a day to prevent extreme hunger.
2. “Food‑Freedom” approach – no foods are off‑limits; this reduces the “forbidden‑fruit” effect.
3. Balanced macros – include protein, healthy fats, and fiber to keep you satiated longer.
Managing Physical Complications
Common complications include sore throat, swollen salivary glands, electrolyte imbalances, and dental erosion. If you notice persistent fatigue, faintness, or irregular periods, contact your GP. Dental health professionals can also help reverse enamel damage if caught early.
Sample 7‑Day Meal Framework
Below is a plain‑text skeleton you can adapt. No specific recipes—just structure:
- Breakfast: Whole‑grain toast + protein (egg or Greek yogurt) + fruit.
- Mid‑morning snack: Handful of nuts or a small smoothie.
- Lunch: Lean protein (chicken, tofu) + veggies + complex carb (quinoa, brown rice).
- Afternoon snack: Veg sticks with hummus or a piece of cheese.
- Dinner: Similar to lunch—vary proteins and veggies for interest.
Self‑Monitoring Tools
Use a simple app or paper journal to record:
- What you ate (no judgment, just facts).
- Urge rating (0‑10) before and after meals.
- Mood notes—are stress, boredom, or loneliness driving cravings?
Levels of Care
Outpatient Therapy
Most people begin here: weekly appointments with a therapist, dietitian visits every 2‑4 weeks, and medication managed by a psychiatrist or GP. This setting works when you’re medically stable and have a supportive environment at home.
Partial Hospitalization & IOP
Partial Hospitalization Programs (PHP) and Intensive Outpatient Programs (IOP) let you attend treatment for most of the day but sleep at home. They’re ideal when you need more structure than weekly visits provide, yet you’re not ready for residential care.
Residential Programs
Residential treatment offers a “home‑like” setting with 24‑hour supervision. It’s useful for those who need longer‑term therapy, nutrition coaching, and a break from triggering home environments. Stays can range from a few weeks to several months.
Inpatient Hospitalization
When physical health is at risk—severe dehydration, electrolyte imbalances, or suicidal thoughts—hospital admission becomes necessary. The goal is rapid medical stabilization before transitioning to a lower level of care.
Decision‑Making Flowchart
Imagine a simple flowchart you can sketch on paper:
- Is your medical status stable? → Yes: Outpatient/Partial Hospitalization. No: Inpatient.
- Do you have strong home support? → Yes: Outpatient. No: Residential.
- Are binge‑purge episodes frequent (≥ 3 times/week) and impairing daily life? → Consider PHP/IOP.
Personal Story Snippet
James (28) was hospitalized after a panic‑induced electrolyte crisis. After a week of IV fluids and medical monitoring, he moved to a residential program where he learned CBT‑E and received daily nutrition counseling. Six months later, he’s thriving in an outpatient setting, attending weekly therapy and managing his meals independently. James credits each level of care for giving him the “steady ladder” he needed to climb out of the disorder.
Balancing Benefits & Risks
Potential Benefits
When therapy, medication, and nutrition work together, you can expect:
- Fewer binge‑purge episodes.
- Improved mood and reduced anxiety.
- Restored physical health—regular periods, stronger teeth, stable weight.
- Better relationships and confidence in social settings involving food.
Possible Risks
Every treatment carries drawbacks:
- Medication side‑effects (sleep changes, nausea).
- Therapy can stir uncomfortable emotions before relief appears.
- Nutrition plans may feel “rigid” initially, triggering anxiety.
- Relapse is possible; it doesn’t mean failure—just a signal to adjust the plan.
Risk‑Mitigation Tips
- Schedule regular check‑ins with your whole care team.
- Keep a crisis plan: emergency contacts, local helpline numbers.
- Track side‑effects in a simple spreadsheet; discuss them promptly.
- Build a “safety net” of supportive friends or online groups.
When to Seek Help Immediately
If you notice any of the following, call emergency services or go to the nearest A&E:
- Severe dizziness, fainting, or heart palpitations.
- Persistent vomiting that leaves you unable to keep fluids down.
- Thoughts of self‑harm or suicide.
Building a Sustainable Recovery Plan
SMART Goal‑Setting
Make goals Specific, Measurable, Achievable, Relevant, and Time‑bound. Example:
- Specific: “I will eat three balanced meals each day.”
- Measurable: “I’ll log meals in a journal.”
- Achievable: “I’ll start with a simple breakfast of oatmeal + fruit.”
- Relevant: “Regular meals reduce binge urges.”
- Time‑bound: “I’ll keep this routine for the next 4 weeks.”
Support Networks
Recovery is rarely a solo journey. Lean on:
- Family members who respect your treatment plan.
- Peer‑support groups—both in‑person (check local listings) and reputable online forums such as Beat or Eating Disorder Hope.
- Therapist‑led groups that focus on skill‑building.
Self‑Care Beyond Treatment
Once the core therapy is under way, layer in activities that nurture your body and mind:
- Gentle yoga or stretching—helps body awareness without calorie counting.
- Mindful walking—use the steps to notice sensations, not thoughts about food.
- Regular sleep schedule—aim for 7‑9 hours to stabilize hormones that affect appetite.
Free Resource Toolkit
Here are a few no‑cost tools you can start using today:
- NHS self‑help CBT booklet (downloadable PDF).
- Beat HelpFinder – locate accredited counsellors near you.
- MyFitnessPal’s free food‑log feature—use it for tracking without judgment.
Conclusion
Effective bulimia treatment isn’t a one‑size‑fits‑all prescription; it’s a personalized blend of therapy, medication, and nutrition that respects both the mind’s complexity and the body’s needs. By understanding how each piece works, weighing benefits against risks, and surrounding yourself with knowledgeable professionals and caring allies, you set the stage for lasting recovery.
If you’re ready to take the first step—whether that’s booking a GP appointment, downloading a trusted self‑help guide, or reaching out to a local support helpline—remember you don’t have to walk this path alone. Your health, your story, and your future are worth the effort. Feel free to share your thoughts in the comments, ask questions, or simply let us know how you’re feeling today. We’re here for you.























Leave a Reply
You must be logged in to post a comment.