Ever wonder if someone you care about is “just drinking a lot” or actually struggling with an addiction? The line can feel blurry, especially when everyday language tosses “addiction” and “substance use disorder” around like synonyms. The truth is a bit more nuanced, and getting that nuance right can change the kind of help you or a loved one gets.
In the next few minutes I’ll walk you through the official definitions, the symptoms you can spot, the real differences between the two terms, and what treatment looks like at every stage. Think of this as a friendly chat over coffee—no jargon, just clear answers and a few real‑life stories to keep things relatable.
What Is SUD?
SUD stands for Substance Use Disorder. It’s the clinical label you’ll find in the DSM‑5 (the Diagnostic and Statistical Manual of Mental Disorders). In plain English, it means a pattern of substance use that causes significant problems or distress over a 12‑month period.
DSM‑5 Criteria (12‑month window)
| # | Criterion |
|---|---|
| 1 | Using larger amounts or for longer than intended |
| 2 | Unsuccessful attempts to cut down or control use |
| 3 | Spending a great deal of time obtaining, using, or recovering |
| 4 | Cravings or strong urges to use |
| 5 | Failure to fulfill major role obligations at work, school, or home |
| 6 | Continued use despite interpersonal problems |
| 7 | Giving up or reducing important activities because of use |
| 8 | Using in physically hazardous situations (e.g., driving) |
| 9 | Use despite known physical or psychological problems |
| 10 | Tolerance (need more for same effect) |
| 11 | Withdrawal symptoms or use to avoid withdrawal |
Count how many of these you see. Two or three = mild SUD, four or five = moderate, six or more = severe. The severity helps clinicians decide how intensive the treatment should be.
Why the 12‑month frame?
Because patterns can fluctuate. A single binge might look alarming, but if it doesn’t repeat over a year it may not meet the disorder’s threshold. The timeframe also respects the idea that people can change—early intervention can keep a mild case from spiraling.
What Is Addiction?
When most people hear “addiction,” they picture someone who can’t stop using a substance, even when they know it’s wrecking their life. That intuition isn’t far off—addiction is essentially the most severe end of the SUD spectrum.
How experts define it
According to the National Institute on Drug Abuse, addiction is a chronic brain disorder marked by compulsive drug seeking, continued use despite harmful consequences, and lasting changes in brain circuitry. It’s not just “bad habits”; it’s a rewiring of the reward system that makes quitting feel almost impossible.
Brain changes in a nutshell
Drugs flood the brain’s dopamine pathways with pleasure signals. Over time the brain adapts—dopamine receptors shrink, tolerance builds, and the person needs more of the drug to get the same buzz. Those changes are why cravings feel like an internal storm you can’t outrun.
A quick story
Maria (a pseudonym) started drinking socially in college. At first it was a few beers on weekends, but after graduating she found herself reaching for a bottle after work to “relax.” Within two years she was drinking daily, had tolerance, and despite a looming divorce and a missed promotion she kept going. Her physician diagnosed her with a severe SUD, and because the pattern matched the addiction definition—compulsive use, loss of control, and major life disruption—her treatment plan focused on both medical detox and long‑term behavioral therapy.
Key Differences Explained
Below is a side‑by‑side look that makes the distinction crystal clear.
| Aspect | Substance Use Disorder | Addiction |
|---|---|---|
| Clinical label | DSM‑5 diagnosis; any severity | Often described as “severe SUD” |
| Primary focus | Number of criteria met | Compulsive use despite major harm |
| Brain impact | Early changes, potentially reversible | Long‑lasting neuro‑adaptations |
| Treatment urgency | Early intervention can prevent progression | Often requires intensive, possibly residential care |
Why does the distinction matter?
Because the right label guides the right help. A person with a mild SUD may benefit from brief counseling and lifestyle tweaks, while someone with full‑blown addiction usually needs a more structured program—detox, medication‑assisted treatment, and ongoing aftercare.
Spotting Substance‑Abuse Signs
Even before a formal SUD diagnosis, there are red flags you can notice in friends or family. Catching them early can make a huge difference.
Physical clues
- Frequent withdrawal symptoms (shakiness, sweating, nausea)
- Rapid weight loss or gain
- Unexplained bruises or injuries
- Changes in appearance—bloodshot eyes, dilated pupils
Behavioral clues
- Secretive behavior or lying about substance use
- Neglecting responsibilities at work or school
- Financial troubles that seem related to buying substances
- Social circles shifting to mostly other users
Psychological clues
- Intense cravings or constant thoughts about using
- Irritability, anxiety, or depression when not using
- Feeling “out of control” about intake
- Using substances as a primary coping mechanism
According to SAMHSA, more than 10 % of U.S. adults reported a substance‑use problem in 2023, and many of those recognized early signs only after a crisis hit.
Addiction Treatment Options
When the line shifts from “problem” to “addiction,” it’s time to explore evidence‑based pathways that actually work.
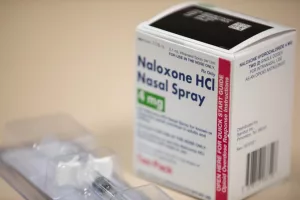
Medication‑Assisted Treatment (MAT)
MAT combines FDA‑approved medications (like buprenorphine, naltrexone, or methadone for opioid use) with counseling. It eases cravings and reduces withdrawal, making it easier to stick with therapy. Research shows MAT can cut overdose deaths by up to 50 %.
Behavioral therapies
- CBT (Cognitive‑Behavioral Therapy) – teaches coping skills to replace substance‑driven thoughts.
- Motivational Interviewing – helps a person resolve ambivalence and commit to change.
- Contingency Management – uses tangible rewards for abstinence milestones.
Residential vs. Outpatient
If cravings are intense or the living environment is triggering, a residential program offers 24‑hour support and a structured schedule. Outpatient care works well for those with milder SUD or strong family support. The choice hinges on severity, safety, and personal responsibilities.
Peer support
Groups like 12‑step meetings, SMART Recovery, or local community circles provide accountability and the “you’re not alone” feeling that science says boosts long‑term success.
Choosing a provider
Ask potential clinicians:
- Are they board‑certified in addiction medicine?
- Do they use evidence‑based protocols (MAT, CBT)?
- What are the insurance and sliding‑scale options?
- Can they tailor treatment to your unique life context?
Prevention & Early Intervention
Stopping a problem before it becomes an addiction is possible, especially with the right community tools.
Community‑based programs
Schools, churches, and local health departments often run educational workshops that demystify substance risks. SAMHSA notes that early‑life education dramatically lowers initiation rates.
Self‑screening tools
Quick questionnaires like the AUDIT (Alcohol Use Disorders Identification Test) or DAST (Drug Abuse Screening Test) can give you a snapshot. Even a five‑minute online quiz can spark a crucial conversation with a doctor.
When to seek help now
- After a single overdose or near‑overdose episode.
- When you or a loved one has tried to quit three times without success.
- If substance use is endangering relationships, employment, or legal standing.
Balancing Benefits & Risks of Knowing the Difference
Understanding the nuanced gap between SUD and addiction does more than satisfy curiosity—it reduces stigma and empowers smarter decisions.
Reducing stigma
When we use precise language (“severe SUD” instead of “just a bad habit”), we acknowledge that the brain is actually fighting the person. That empathy makes it easier for someone to admit they need help.
Avoiding over‑medicalization
Not every heavy drinker is addicted. Over‑labeling can push people into unnecessary treatment, while under‑labeling can leave them untreated. The balanced view keeps care proportional to need.
Empowered decision‑making
Families and clinicians alike can craft a plan that matches the actual severity—whether that’s a brief motivational interview, a six‑month outpatient program, or a full residential stay.
Conclusion
To sum it up, substance use disorder is the umbrella term that captures any problematic pattern of use, measured by specific DSM‑5 criteria. Addiction lives at the furthest end of that spectrum—a severe, compulsive condition where the brain’s reward system has been hijacked.
Spotting early substance‑abuse signs and understanding the difference between a mild SUD and full‑blown addiction can guide you toward the right level of help—whether that’s a quick self‑screen, a brief counseling session, or a comprehensive addiction treatment plan.
If any of this resonates with you, take the next step: run a short screening quiz, talk to a trusted health professional, or explore your local resources on FindTreatment.gov. Remember, reaching out isn’t a sign of weakness; it’s a brave move toward a healthier, more balanced life. Got questions or a story to share? Drop a comment below—let’s keep the conversation going and support each other on this journey.




















Leave a Reply
You must be logged in to post a comment.