Bulimia relapse is the moment when someone who’s been working toward bulimia recovery finds themselves slipping back into binge‑and‑purge patterns. It’s frustrating, scary, and it can feel like a personal failure—but it’s also a normal part of the healing journey. Recognizing that a relapse is a signal, not a verdict, can change the entire conversation.
In the next few minutes we’ll walk through exactly what a relapse looks like, why it happens, how to spot the early warning signs, and – most importantly – what practical steps you can take right now to get back on track. Grab a cup of tea, settle in, and let’s talk it through like friends.
What Is Relapse?
How do clinicians define a bulimia relapse?
According to bulimia.com, a relapse is typically measured when a person experiences two or more binge‑purge episodes per month for at least two consecutive months. This pattern meets the DSM‑5 criteria for bulimia nervosa again, meaning the disorder has officially resurfaced.
Is a relapse the same as a lapse?
A “lapse” is usually a single, isolated incident—maybe an unexpected binge at a holiday dinner. A lapse often resolves quickly, and the person can return to their recovery plan without major disruption. A relapse, on the other hand, involves a repeated pattern that signals the underlying coping mechanisms have been re‑triggered.
Quick comparison
| Term | Frequency | Typical Duration | Clinical Meaning |
|---|---|---|---|
| Lapse | 1‑2 isolated episodes | Days‑weeks | Minor setback, easy to re‑enter recovery |
| Relapse | ≥ 2 episodes/month for ≥ 2 months | Weeks‑months | Return to diagnostic criteria |
| Full remission | < 2 episodes/month | > 12 months | Meets recovery standards |
Warning Signs
Behavioral red flags
When the pattern shifts, the first clues are often actions you can see:
- Skipping meals or eating in secret.
- Counting calories obsessively (e.g., writing “good” vs. “bad” food lists).
- Finding yourself bingeing alone, then feeling the urge to purge.
- Increasingly frequent mirror checks or daily weighing.
Thoughts and emotions that signal trouble
Negative self‑talk is a silent engine that fuels the cycle. You might notice:
- Constant self‑criticism (“I’m so weak,” “I’ll never be thin enough”).
- Intense shame after any eating, even if it was a balanced meal.
- Racing thoughts about weight loss or “perfecting” your body.
Physical cues you shouldn’t ignore
Our bodies sometimes scream before our minds catch up. Look for:
- Rapid weight fluctuations (often a gain from bingeing, then a loss from purging).
- Dental enamel erosion or swollen throat—signs of frequent vomiting.
- Excessive fatigue from erratic eating patterns.
10 Early‑Warning Signs Checklist
- Secretive eating or binge episodes.
- Skipping or drastically restricting meals.
- Obsessive calorie tracking.
- Frequent weighing or mirror checking.
- Negative self‑talk about body/food.
- Increased isolation around meals.
- Sudden urges to exercise excessively.
- Physical signs: enamel wear, sore throat.
- Heightened anxiety or depression.
- Loss of interest in treatment appointments.
Common Triggers
Life events that can tip the balance
Stressful milestones often act like matchsticks in a dry forest. According to bulimia.com, common stressors include:
- Moving to a new city or starting a new job.
- Major loss—death of a loved one, divorce, or breakup.
- Life transitions like getting married, having a baby, or returning to school.
- Holidays, where food takes center stage and old patterns feel comforting.
How stress translates to binge urges
When cortisol spikes, the brain’s reward pathways light up—similar to how addictive substances work. A study highlighted by Monte Nido explains that stress can re‑activate the dopamine surge that originally made disordered eating feel soothing, pulling you back toward familiar (but unhealthy) coping tools.
Food‑related and environmental triggers
It’s not just big events. Even the smell of a favorite bakery, scrolling through “clean‑eating” Instagram feeds, or attending a party where you feel judged can spark cravings. The key is to notice when a specific place, person, or food becomes a mental “alarm bell.”
Short stories, real‑world examples
Anna*, a 24‑year‑old graduate student, thought she’d left bulimia behind after a year of therapy. When her semester load doubled, she found herself skipping meals between classes, then bingeing on pizza late at night. The stress of deadlines re‑awakened the old binge‑purge cycle.
Mark*, a 32‑year‑old accountant, noticed his relapse after his partner suggested a “diet‑focused” vacation. The constant talk about calories made him feel as though he was back in the “weight‑obsessed” mindset that first triggered his disordered eating.
Prevention Strategies
Creating a personalized relapse‑prevention plan
The most powerful tool is a written plan you can pull out the moment you feel shaky. A typical layout includes:
- Triggers: List situations, foods, emotions that raise red flags.
- Warning signs: Your personal checklist (the 10‑point list above).
- Support contacts: Therapist, trusted friend, dietitian, crisis line.
- Quick‑action steps: Call a supporter, schedule an extra therapy session, practice a grounding exercise.
Sticking to treatment
Regular check‑ins with your therapist or psychiatrist are non‑negotiable. Skipping appointments, cutting back on medication, or ignoring nutrition counseling dramatically raises relapse risk, as noted by bulimia.com. Think of appointments as the oil changes that keep your recovery engine running smoothly.
Effective coping skills
Several evidence‑based techniques have shown strong results for bulimia:
- CBT‑E (Cognitive‑Behavioral Therapy‑Enhanced): Challenges the “all‑or‑nothing” thoughts that fuel binge urges.
- DBT distress‑tolerance: Uses sensory grounding (“5‑4‑3‑2‑1” technique) to ride out emotional spikes.
- Mindful eating: Slows down the process, helping you notice true hunger vs. emotional cravings.
- Physical activity with limits: Regular, moderate exercise (30‑45 minutes, 3‑5 times a week) without using it as punishment.
My 7‑Day Relapse‑Prevention Worksheet (template)
| Day | Trigger(s) | Warning Sign(s) | Action Plan |
|---|---|---|---|
| Mon | Work deadline | Skipping lunch | Pack balanced snack; call therapist if anxiety spikes |
| Tue | Holiday party | Pre‑meal anxiety | Practice deep breathing; bring a supportive friend |
| Wed | Social media diet posts | Calorie counting | Limit scrolling; replace with a hobby |
| Thu | Family argument | Negative self‑talk | Write affirmations; reach out to support person |
| Fri | Empty fridge | Sudden binge urge | Meal‑prep for weekend; call dietitian |
| Sat | Quiet evening alone | Isolation | Join a peer‑support call |
| Sun | Reflection on week | Over‑analysis | Journal successes, schedule next week’s therapy |
What to Do If a Relapse Happens
First steps: self‑compassion and outreach
Take a deep breath. You haven’t failed; you’ve simply hit a bump. The most helpful first move is to reach out—text your therapist, call a trusted friend, or use a crisis line. According to the National Eating Disorders Association, early contact can shorten the duration of a relapse from weeks to a few days.
Rebuilding momentum
Once you’ve disclosed the slip, set a tiny, achievable goal for the next 24 hours—perhaps a regular breakfast or a brief therapy check‑in. Small wins rebuild confidence faster than trying to “make up” for the whole setback.
When to consider a higher level of care
If you notice any of the following, it may be time for intensive outpatient or inpatient support:
- Frequent vomiting (more than three times a day).
- Severe electrolyte imbalance or dizziness.
- Inability to keep meals down for 48 hours.
- Intense thoughts of self‑harm tied to body image.
Relapse Response Flowchart (step‑by‑step)
- Notice warning sign →
- Practice grounding (5‑4‑3‑2‑1) →
- Contact support person →
- Schedule rapid therapy session (within 48 h) →
- Review nutrition plan and adjust meals →
- Monitor for physical complications; seek medical care if needed.
Treatment & Recovery Options
Therapies with strong relapse‑prevention data
Beyond CBT‑E, these modalities are frequently recommended:
- Family‑Based Therapy (FBT): Engages loved ones as part of the recovery team.
- Interpersonal Psychotherapy (IPT): Focuses on relationship patterns that may trigger binge cycles.
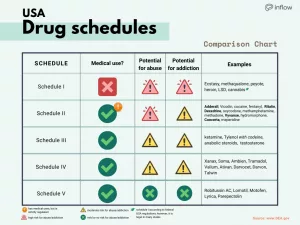
- Medication: Fluoxetine (Prozac) has FDA approval for bulimia and can reduce binge urges when paired with therapy.
- Nutrition counseling: Teaches balanced meal planning to avoid extreme hunger—a primary binge trigger.
Finding qualified professionals
You can locate certified eating‑disorder specialists through the National Eating Disorders Association’s treatment finder. Look for clinicians with credentials in CBT‑E, registered dietitians experienced with eating disorders, and psychiatrists familiar with fluoxetine dosing.
Support groups—peer or clinician led?
Both have merits. Peer groups offer shared lived experience—often the “you’re not alone” moment that breaks isolation. Clinician‑led groups provide structured skill‑building. Many people benefit from attending a hybrid of both types.
Treatment Options vs. Relapse‑Prevention Effectiveness
| Option | Relapse‑Prevention Strength | Typical Duration |
|---|---|---|
| CBT‑E | High | 20‑30 weeks |
| Family‑Based Therapy | Medium‑High | 3‑6 months |
| Medication (Fluoxetine) | Medium | Ongoing |
| Peer Support Group | Medium | Weekly/ongoing |
| Nutrition Counseling | High | 12‑16 weeks |
Expert Insight & Real‑World Experience
What clinicians say
Dr. Amy Baker, PhD, FAED, notes, “Relapse is a data point, not a verdict. It tells us where the safety net slipped, and we can patch it together.” Her perspective underscores the importance of viewing each setback as actionable information rather than a personal flaw.
Personal story: learning from a slip
When I was 27, I thought I’d finally beaten bulimia after two years of therapy. A stressful move to a new city knocked me off balance. I found myself binge‑eating on midnight pizza, followed by a wave of guilt. I called my therapist within 24 hours, wrote down my triggers, and started a daily “check‑in” journal. Within a month, the binge frequency dropped from three times a week to zero. The lesson? Rapid honesty beats silent shame every time.
Moving Forward With Hope
Bulimia relapse can feel like a storm crashing through calm waters, but the good news is that storms pass. By staying aware of warning signs, knowing your personal triggers, and having a concrete action plan, you turn a potential setback into a stepping stone toward deeper recovery.
Remember, you’re not alone. Reach out to a therapist, a supportive friend, or a trusted helpline the moment a doubt surfaces. Your journey is uniquely yours, but the tools we’ve discussed are universal—use them, adapt them, and keep moving forward.
What’s your next small step? Maybe it’s writing down today’s trigger, scheduling that overdue therapy session, or simply sharing this article with someone who might need it. You’ve got this.























Leave a Reply
You must be logged in to post a comment.