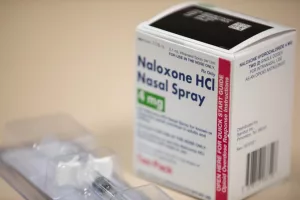
Most people don’t realize that the number of naloxone kits you can get each month isn’t just a random number—it’s a policy decision that can literally mean the difference between life and death. In the next few minutes, I’ll walk you through why those limits exist, how they differ by insurance, and what you can actually do if you hit a ceiling. Think of this as a friendly chat over coffee, with a dash of real‑world data and a sprinkle of empathy.
Quick Answer Summary
If you’re wondering, “How many nasal sprays can I get?” the short answer is: most plans allow 2–4 sprays per 30 days, but the exact figure varies by carrier, state standing order, and whether you’re using a prescription or buying over‑the‑counter. Those limits matter because a second dose often saves a life when the first one isn’t enough.
What Are Limits
In health‑care lingo, a “quantity limit” (sometimes called a “max‑day supply”) means the maximum number of units a pharmacy can dispense for a single prescription or benefit period. For naloxone, the unit is typically a pre‑filled nasal spray (4 mg) or a 0.4 mg injectable vial.
These limits are written into pharmacy benefit manager (PBM) contracts and, in many states, into standing‑order laws. For example, Montana’s 2022 standing order explicitly requires pharmacists to designate a minimum quantity of 2 sprays per prescription, but it also leaves room for providers to write larger amounts if they deem it necessary.
Why Plans Impose
At first glance, “why would they limit a life‑saving drug?” you might ask. The short answer is cost control, but let’s unpack that a bit.
- Budget Management: Insurers negotiate drug prices with manufacturers. Setting a cap helps keep the overall spend predictable.
- Safety Concerns (Myths vs. Facts): Some fear over‑use, but studies consistently show that increased availability does not lead to higher rates of misuse. Instead, broader access correlates with lower overdose mortality.
- Balancing Public‑Health Goals: By limiting quantities, plans aim to distribute the drug to a larger pool of people, assuming each person only needs one dose. Unfortunately, real‑world overdose scenarios often need a second or third spray.
Imagine a classroom where the teacher hands out only one notebook per student, assuming everyone will use it the same way. Some kids will need extra paper, but the rule doesn’t bend. That’s essentially what some insurers are doing with naloxone.
Limits By Insurance
Not all plans are created equal. Below is a quick snapshot of how the most common insurance types handle naloxone quantity limits.
- Commercial PPO / HMO: Typically 2–4 sprays per 30 days. Some carriers allow an extra injectable if you already have the nasal spray.
- Medicare (Part D) & Medicaid: Many state Medicaid programs waive limits for “high‑risk” members (e.g., those on high‑dose opioids). Medicare Advantage often mirrors commercial plans but may have “no limit” clauses for OTC purchases.
- Employer‑Sponsored / Self‑Pay: If you buy OTC, you usually sidestep the prescription benefit, meaning no formal limit—but the price can be higher.
For a deeper dive into what your specific plan might cover, check out our guide on naloxone coverage. Knowing the fine print can save you a lot of hassle later.
Impact On Overdose
Quantity limits aren’t just a bureaucratic footnote—they have real consequences. In 2023, a study published in the Journal of Public Health Policy found that states with more generous naloxone dispensing rules saw a 12 % reduction in opioid‑related deaths compared with states that capped dispensing at one spray per prescription.
Let me tell you a quick story. A friend of mine, Maya, works at a community health center. One night, a neighbor overdosed on fentanyl. Maya gave the first nasal spray, but the person didn’t wake up. She needed a second dose. Unfortunately, Maya’s insurance had a “2‑spray per month” limit, and she’d already filled the pair earlier that week for a family member. She called the pharmacy, fought a prior‑authorization battle, and eventually got an extra kit—but not before 20 agonizing minutes had passed. Maya still shakes when she thinks about it.
That anecdote underscores why the “94 % of plans cover at least one generic injectable or a 4‑mg spray” statistic (as noted in the reference meta description) is encouraging, yet the remaining 6 % of plans could be the difference between life and loss, especially in rural areas where EMS response times are longer.
Navigate The Limits
Good news: you don’t have to sit helplessly while the system decides how many doses you can hold. Here are actionable ways to push past those caps.
- Prior Authorization (PA): Call your plan’s member services and ask for a “high‑risk exemption.” Many insurers approve a PA if you or a household member is on high‑dose opioids (≥ 50 MME/day) or if you’ve had a recent overdose.
- Standing‑Order Pharmacies: Some states, like Montana and Colorado, let any pharmacist dispense naloxone without a prescription and without a formal limit. Find a local pharmacy that participates in the state’s naloxone access program.
- Combine Forms: Use one nasal spray and one 0.4 mg injectable. Because many plans count them separately, you can safely have two doses on hand without hitting a single product limit.
- Community Distribution Kits: Non‑profits and health departments often give away kits for free or at a reduced price. Those kits are typically exempt from insurance limits.
Remember, every time you ask for a PA or use a standing order, you’re not just getting a spray for yourself—you’re also sending a message that our health system should prioritize access over arbitrary numbers.
Plan Limits Table
| Plan Type | Nasal Spray Limit | Injectable Limit | OTC Exception | Notes / Exemptions |
|---|---|---|---|---|
| Commercial PPO/HMO | 2–4 per 30 days | Unlimited (if separate) | None (counts toward total) | Prior‑auth possible for >2 |
| Medicare Part D | 3 per 30 days | 1 per 30 days | OTC not counted | High‑risk exemption under CMS guidance |
| State Medicaid | Unlimited in most states | Unlimited | OTC not applicable | Waived for chronic pain patients |
| Employer‑Sponsored | 2 per 30 days | 1 per 30 days | OTC purchases unrestricted | Depends on company PBM |
Verify Your Limits
Feeling a bit overwhelmed? Here’s a simple, step‑by‑step guide to find out exactly what your plan allows.
- Log into your pharmacy benefits portal. Look for the “Formulary” or “Drug Details” tab.
- Search “naloxone.” You’ll see a line that says “Maximum quantity per prescription” or “Maximum fills per month.”
- Call member services. Phrase your question like this: “Can you tell me the quantity limit for naloxone nasal spray under my plan?” Write down the representative’s name and reference number.
- Document the response. A screenshot or email confirmation will be handy if you need to submit a prior‑authorization.
- Ask about exemptions. If you’re on high‑dose opioids, ask if you qualify for a “high‑risk” exception. Many carriers will lift the limit with a simple doctor’s note.
Doing this homework once can prevent a frantic night of scrambling for a second dose.
Final Thoughts Here
Understanding naloxone quantity limits isn’t just an academic exercise—it’s a matter of personal safety and community health. The limits exist, but they’re not set in stone. With a little knowledge, a quick phone call, and the willingness to use standing‑order pharmacies or community programs, you can make sure you always have enough naloxone on hand.
We’ve covered the why, the how, and the what‑next. If you’ve learned something new, great! If you still have questions, you’re not alone—reach out to a pharmacist you trust, or explore our resources on naloxone restrictions, opioid overdose reversal, and naloxone access. Knowledge empowers us all to act confidently when seconds count.






















Leave a Reply
You must be logged in to post a comment.