Narcolepsy is a neurological disorder that disrupts the sleep–wake rhythm, causing powerful urges to sleep at inappropriate times during the day and night. Sleep apnea involves interruptions in breathing while you’re asleep.
With narcolepsy, you might suddenly fall asleep during routine activities like speaking or eating. Sleep apnea usually stems from a physical blockage in the throat, though it can also arise from neurological dysfunction.
Although both are sleep disorders, their signs and treatments differ markedly.
Read more about narcolepsy and sleep apnea.

What are the symptoms of narcolepsy and sleep apnea?
Both conditions can produce excessive daytime sleepiness, but for distinct reasons.
Sleep apnea
Sleep apnea causes breathing to stop intermittently during sleep. These pauses can range from a few seconds to several minutes.
Sleep apnea is divided into three types based on the root cause:
- Obstructive sleep apnea: Occurs when tissues in the mouth or throat block the airway during sleep.
- Central sleep apnea: Happens when the brain’s signaling to breathe is disrupted.
- Complex sleep apnea: A mixed form featuring both obstructive and central elements.
Common signs of sleep apnea can include:
- marked daytime drowsiness due to poor restorative sleep
- frequent loud snoring
- gasping or choking while asleep
- waking multiple times during the night
- dry mouth or headache upon waking
- reduced sexual desire or dysfunction
- frequent nighttime urination
Narcolepsy
Typical features of narcolepsy may include:
- Excessive daytime sleepiness: Individuals with narcolepsy have abrupt “sleep attacks” and can nod off without warning for seconds to minutes.
- Cataplexy: A sudden loss of muscle tone, which can be mild (eyelid drooping) or more severe and cause collapse.
- Sleep paralysis: Brief inability to move when falling asleep or waking is common in narcolepsy.
- Hallucinations: Vivid, often visual hallucinations can occur at sleep onset or during naps.
- Fragmented nocturnal sleep: Many people with narcolepsy have trouble maintaining sleep at night despite daytime sleepiness.
- Automatic behavior: People may continue an activity while partly asleep—such as talking or eating—without later memory of it.
What causes narcolepsy and sleep apnea?
Both disorders have multiple possible causes.
Sleep apnea causes
Obstruction of the airway or neurologic problems can lead to sleep apnea. Contributing risk factors include:
- overweight or obesity
- enlarged tonsils
- endocrine disorders such as hypothyroidism, acromegaly, or polycystic ovary syndrome (PCOS)
- chronic pulmonary diseases like asthma or COPD
- heart failure
- kidney failure
- certain genetic syndromes, such as Down syndrome or cleft palate
- neuromuscular conditions, for example stroke, myotonic dystrophy, or dermatomyositis
- pregnancy
Narcolepsy causes
Narcolepsy is categorized as type 1 or type 2; type 1 includes cataplexy, while type 2 does not.
Nearly all individuals with type 1 narcolepsy have reduced levels of the neuropeptide hypocretin (also called orexin), which helps regulate wakefulness and sleep. Factors that may lead to low hypocretin include:
- autoimmune disorders
- hereditary or genetic influences
- head trauma
The origins of type 2 narcolepsy remain largely unclear.
Can sleep apnea cause narcolepsy, or the reverse?
Researchers continue to explore connections between narcolepsy and sleep apnea. Current evidence suggests that people with narcolepsy may have a higher prevalence of obstructive sleep apnea compared with those without narcolepsy.
An increased body mass index (BMI) in people with narcolepsy might play a role. Similarly, studies show a strong link between obesity and obstructive sleep apnea. A BMI of 30 or above is considered obese, while a BMI below 25 is considered within a normal range.
A 2018 study noted that obstructive sleep apnea was the most frequent medical condition among 68 people with narcolepsy in Olmsted County, Minnesota. There’s little evidence indicating the reverse relationship.
Further investigation is required to clarify how the two conditions influence each other.
Can you have both narcolepsy and sleep apnea?
Yes—an individual can be diagnosed with both disorders simultaneously. Coexistence of both conditions can complicate diagnosis and management.
What other conditions can cause daytime drowsiness and fatigue?
Many conditions besides narcolepsy and sleep apnea can produce daytime sleepiness. Other possible causes include:
- insufficient sleep for any reason
- medications such as sedatives, beta-blockers, antihistamines, anticonvulsants, antidepressants, or opioids
- hypothyroidism
- insomnia
- overactive bladder
- depression
- anxiety disorders
- poor nutrition
- brain injuries
- other sleep disorders, like restless legs syndrome
How are sleep apnea and narcolepsy treated?
Treatment depends on the underlying causes and the patient’s overall health.
Sleep apnea
Therapies for sleep apnea focus on restoring airflow during sleep and addressing contributing conditions. Options include:
- weight-loss programs
- continuous positive airway pressure (CPAP) devices
- bilevel positive airway pressure (BiPAP) machines
- sleeping on your side
- oral appliances
- surgical procedures to reduce upper airway obstruction or implantation of pacemaker-like devices to stimulate nerves controlling the tongue
Learn about home remedies for sleep apnea.
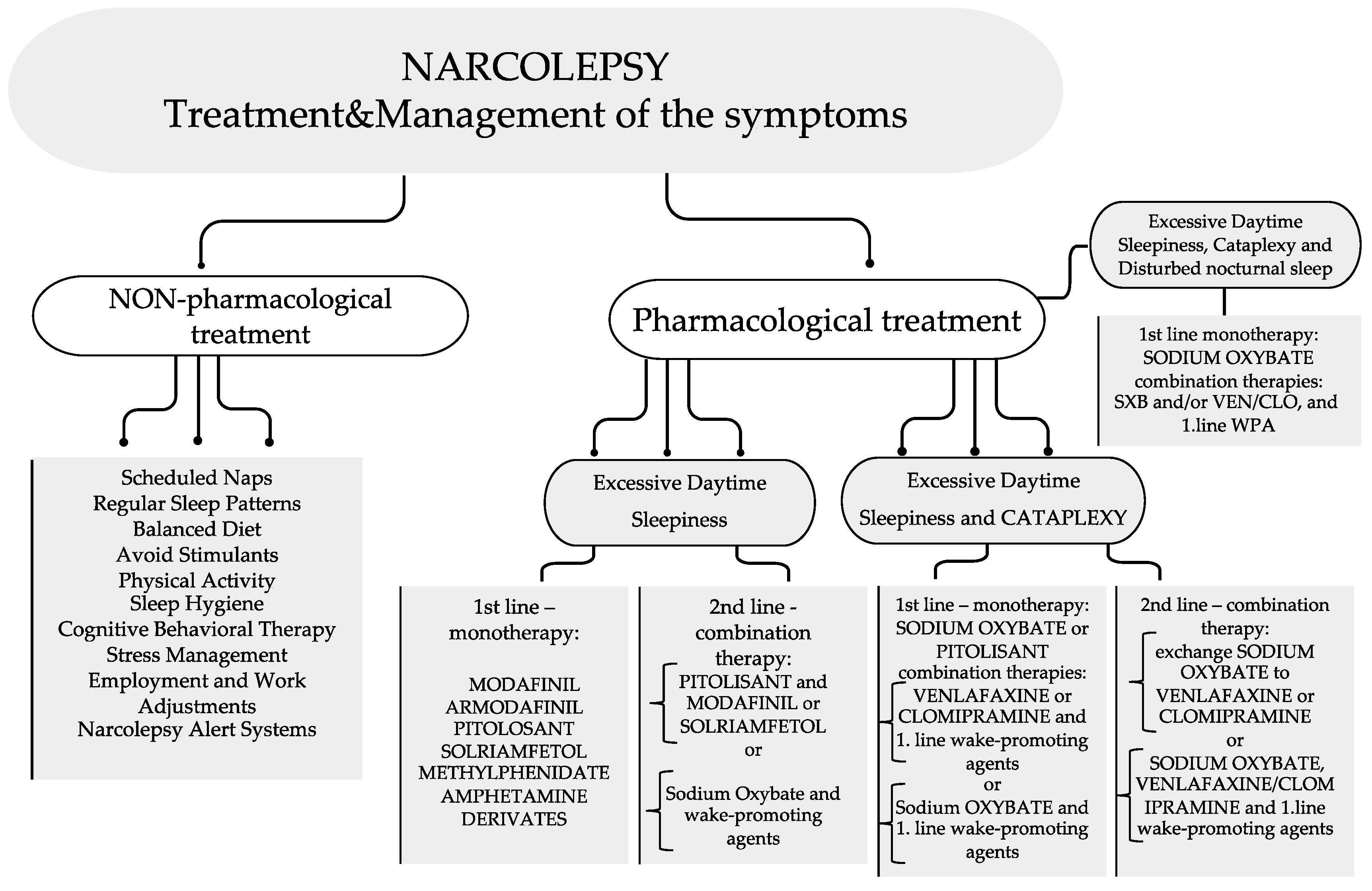
Narcolepsy
Narcolepsy treatment emphasizes lifestyle adjustments and medications.
Helpful lifestyle measures include:
- scheduling brief naps when feasible
- keeping a consistent sleep–wake routine
- avoiding alcohol and caffeine, especially near bedtime
- quitting tobacco
- regular daily exercise
- avoiding heavy meals before sleep
- practicing relaxation techniques at night
Medications that may be used include:
- modafinil
- amphetamine-like stimulants
- pitolisant (Wakix)
- solriamfetol (Sunosi)
- antidepressants
- sodium oxybate
How do clinicians diagnose sleep apnea and narcolepsy?
Evaluation for either disorder starts with a visit to a primary care provider. A physical exam and review of medical history are initial steps. If a sleep problem is suspected, you may be referred to a sleep specialist for further testing.
The gold standard test for obstructive sleep apnea is polysomnography. This overnight study at a sleep center or hospital records:
- blood oxygen changes via pulse oximetry
- airflow at the nose and mouth
- respiratory effort
- brain activity via electroencephalogram (EEG)
- eye movements via electrooculogram (EOG)
- heart rate and rhythm via electrocardiogram (ECG)
- muscle activity via electromyography (EMG)
Polysomnography also aids narcolepsy diagnosis. Another test used is the multiple sleep latency test, which measures how quickly you fall asleep. In some patients, doctors may analyze hypocretin levels in cerebrospinal fluid obtained by a spinal tap.
Learn more about tests for narcolepsy and tests for sleep apnea.
When should you see a doctor?
Consult a healthcare professional if you suspect a sleep disorder.
Narcoleptic sleep attacks can raise the risk of accidents and injuries. Sleep apnea is associated with major chronic health problems.
The takeaway
Narcolepsy is defined by sudden, uncontrollable sleep episodes that can occur anytime, while sleep apnea is defined by breathing interruptions during sleep.
If you suspect either condition, see a clinician for evaluation and treatment to reduce the risk of complications. For additional related information, you may also find resources on a narcolepsy service dog and the connection between tinnitus and sleep apnea helpful.
























Leave a Reply
You must be logged in to post a comment.