Many causes of penile color changes are benign, including sexual arousal, bruising, and common dermatologic issues. Less frequent but more serious causes include lichen sclerosus and penile cancer, though the latter is uncommon.
During sexual arousal, increased blood flow to the penis can give it a reddish to purplish hue as vessels and the glans engorge with blood. However, there are other potential explanations for a penis shifting to an altered color that warrant attention.
Causes of penis discoloration vary widely — from a zipper-induced contusion to penile cancer, a rare disease that makes up under 1% of cancers in people with a penis. Sometimes a color change signals a sexually transmitted infection (STI) or a noninfectious, harmless skin change.
Any notable penile discoloration is typically worth medical assessment. Often it will be temporary and not serious, but self-diagnosis is not recommended.
If the color change stems from a significant underlying condition, obtaining a diagnosis and beginning treatment early is the prudent course.
Below are possible causes and common treatment approaches for discoloration of the penis.
Bruise or trauma
A bruise forms when tiny blood vessels just beneath the skin rupture, depositing blood that shows as discoloration. On the penis, a bruise can follow a zipper mishap, particularly vigorous sex or masturbation, or being pinched or struck.
Minor bruises typically darken during healing and then gradually fade.
Treatment
Applying warm compresses can help disperse pooled blood and speed healing of a bruise. Many mild injuries don’t require medical care, but more severe contusions should be evaluated by a clinician. Likewise, a small bruise that fails to resolve on its own deserves medical review.
To reduce the risk of traumatic injury to the penis, wear appropriate protective equipment during sports and take care when fastening pants.
Penile melanosis
Penile melanosis is a benign pigmentary change that produces small darker patches on the shaft or glans of the penis. It results from localized concentrations of melanin within the skin.
Penile melanosis is not an STI and is not transmissible.
The precise reason some men develop this condition isn’t well established. There is some evidence, however, that psoriasis therapy involving psoralen plus ultraviolet light may elevate the likelihood of penile melanosis.
Treatment
Typically no treatment is required, though in select cases surgical excision of the patches may be an option. Be aware that removal can leave visible scarring.
For more information, see resources on penile melanosis.
Contact dermatitis
Contact dermatitis is an inflammatory skin reaction that occurs after exposure to an irritant or allergen. Soaps, detergents, and personal care products can trigger this reaction on any skin surface.
When it affects the penis, a common culprit is latex in condoms. A person might not realize they have a latex sensitivity until they have a reaction, which can cause red, itchy skin. Severe reactions may break the skin and produce serum discharge.
Other triggers include fragrances, preservatives, or ingredients in soaps and laundry products.
Treatment
Mild contact dermatitis can often be managed with over-the-counter topical corticosteroid creams. If the skin is broken, see a healthcare provider to reduce the risk of secondary infection. If you have latex sensitivity, nonlatex condoms are available as an alternative.
Lichen sclerosus
White, thin patches on the penis may indicate lichen sclerosus, a chronic skin disorder that is more frequently seen in uncircumcised individuals.
Besides expanding pale areas, affected penile skin can become fragile and itchy. Symptoms may include painful erections and reduced urinary flow.
Lichen sclerosus is a long-term condition that can cycle between flare-ups and remission.
The exact cause remains unclear. A family history can raise risk, and autoimmune mechanisms — where the immune system attacks healthy tissue — are suspected contributors.
Those with lichen sclerosus may have increased likelihood of other autoimmune disorders, such as thyroid disease or vitiligo.

Treatment
Standard therapy often involves potent topical steroid ointments applied to the affected skin. If the foreskin is the main site of disease, circumcision may be recommended.
Lichen planus
Lichen planus can produce flat purple or white lesions, frequently with ringlike borders, on the penile tip. It may present as itchy papules, and in some people painful ulcers can form.
Prompt medical attention is important because lichen planus can cause complications and may raise the risk of certain cancers.
Treatment
Some people have lichen planus without symptoms, in which case aggressive therapy might not be needed.
Topical corticosteroids can lessen inflammation and itching. Severe or resistant cases may require more potent systemic treatments or consideration of circumcision.
Vitiligo
Vitiligo happens when pigment-producing cells (melanocytes) stop making melanin, the pigment responsible for skin color. Although it commonly affects areas like elbows and knees, vitiligo can occur anywhere, including the penis. It’s neither painful nor contagious, and the skin texture usually remains normal.
Vitiligo may appear as a small pale spot or involve a much bigger region.
Treatment
Topical steroids and some immune-modulating medications can help restore pigment in smaller or milder patches.
Syphilis
Syphilis is a sexually transmitted bacterial infection that, if untreated, can later affect the brain, heart, and other organs.
The earliest sign is often a single painless ulcer — red or pale — on the penis. If not treated, a widespread, sometimes itchy rash may develop on the penis and elsewhere on the body. Additional symptoms can include headache, fever, and fatigue.
Other STIs, such as genital warts, can also alter the appearance of the genital skin with bumps or growths. Regular STI testing facilitates early treatment when infections are present and helps prevent transmission. Practicing safer sex reduces the likelihood of acquiring STIs.
Treatment
Syphilis is treated with appropriate antibiotics, most commonly penicillin. Successful treatment does not prevent future reinfection if exposed again through unprotected sex with an infected partner.
Penile cancer
Although penile cancer is uncommon, recognizing warning signs is important so you can act quickly.
An early sign can be a color change of the penile skin, involving the shaft or glans. The penis may appear reddened, or flat brown lesions can develop. The affected skin may thicken and feel tender.
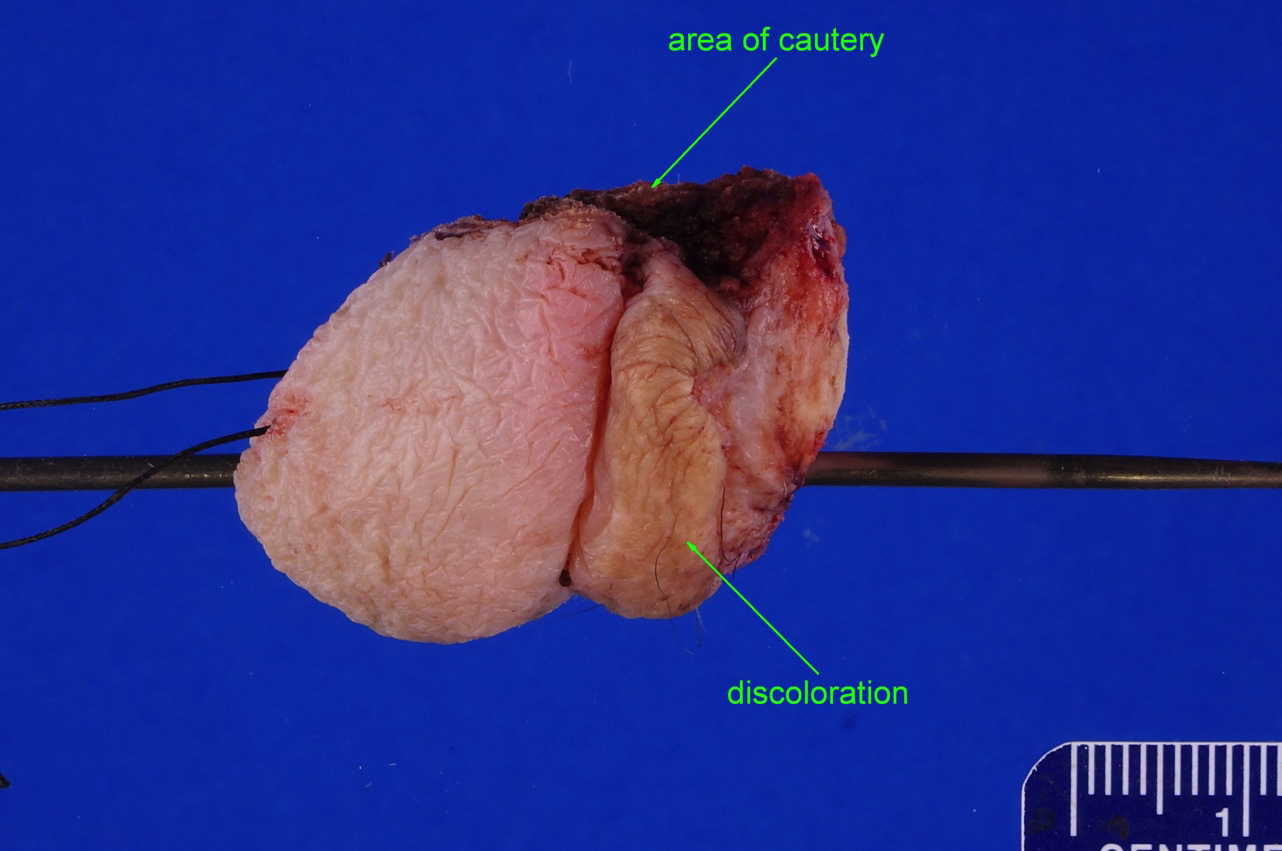
Treatment
Treatment options include radiation or surgical removal of cancerous skin in localized cases. The extent and character of the tumor determine the optimal treatment plan.
When to seek care for penis discoloration
If you notice any penile color change other than a mild bruise with a known cause, you should consult your primary care doctor or a urologist. Urologists specialize in the urinary system and male reproductive organs.
Diagnosis usually begins with a physical exam and review of your medical history and symptoms.
Depending on suspected causes, blood tests and other diagnostic studies may be ordered.
Common initial lab work includes a complete blood count, which measures:
- white blood cells
- red blood cells
- platelets
Elevated white blood cell counts, for example, indicate the body is fighting infection. Blood tests can also screen for STIs like syphilis, HIV, herpes, and hepatitis, and sometimes detect markers suggestive of cancer.
Suspicious sores or growths may be biopsied — a small tissue sample is taken and examined microscopically. Biopsy results can identify cancerous cells or other disease processes.
Takeaway
Any noticeable change in the appearance of your penis, particularly unusual discoloration, patches, or growths, can be distressing. Don’t delay seeking medical evaluation. Early recognition and treatment can reduce the risk of complications from an untreated condition.
If a harmless but lasting color change occurs, you may find it helpful to speak with a mental health professional to help adjust to the change.
























Leave a Reply
You must be logged in to post a comment.