“Hmm, why is my toddler gaining weight so fast? Is this normal?”
Let’s cut to the chase. If you’re worried your child’s BMI might not fit the “status quo,” you’re not alone. But here’s the twist: 2025’s newest research says there are two main childhood BMI trajectories you should know about—even if the words “low stable” or “median stable” sound like alphabet soup. And guess what? These patterns start way before birth. Let’s unpack this together.
Imagine 9,400 kids followed from toddlerhood to pre-adolescence. A Washington State University study found two distinct paths: some kids’ BMIs climb steadily, while others veer into “atypical” territory. By age 3.5, those off-track? Yeah… they’re way more likely to hit the 95th percentile (obesity range) by age 9. But wait—before you freak out over percentages, let’s chat about why BMI is like a guessing game for kids. Ready?
What’s the “Real” Story Behind Childhood BMI Patterns?
It’s Not Just Genetics… Your Body Composition Changes Like the Weather
Kids aren’t just mini adults. Their bodies morph—literally—as they grow. Like the seasons shifting, a toddler’s BMI peaks, dips, then spirals upward again. Puberty messes with the numbers. Muscle? Fat? Growth spurts? They all blur the lines. One raw fact from NCBI: “BMI’s association with health risk varies by age, sex, and ethnicity” (NCBI). Translation: your child’s BMI report might not tell you what’s really going on inside their body.
Picture this. A kid who’s a sports nut and muscular might clock a “high” BMI. Meanwhile, another child eats salads every day but carries extra fat. Same number, different stories. That’s why experts like the Cleveland Clinic say mom and dad’s weight (more on that later!) and lifestyle play such a role (Cleveland Clinic).
Key Terms to Know
Before we jump in:
- Low stable: Maintains a healthy range (5th–85th percentile).
- High rising: Spikes into overweight/obesity zones by age 10.
- Body fat distribution: Where the fat settles in the body (belly vs. limbs). Doesn’t show up on BMI.
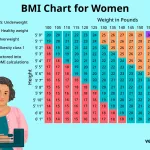
Quick Tip: Pediatric BMI Charts Aren’t Like Adult Metrics
| Class | BMI Percentile |
|---|---|
| Underweight | < 5th |
| Healthy Weight | 5th–85th |
| Overweight | 85th–95th |
| Obese | ≥95th |
Why does this matter? Because a child growing up isn’t the same as a child growing within their percentile. Confusing, right? Let’s simplify.
The Real Links Between Prenatal Factors & Toddler Growth
Mom’s Health Sets the Stage
We all know pregnancy is a big deal for Baby. But how much does it shape their BMI years later?
“Wow.” That’s what happened to a mom named Lisa we spoke to. She had diabetes during pregnancy. By age 3, her daughter was hovering near the 90th percentile and flashing irksome heart health red flags. Enter 2025’s ECHO Program data: prenatal factors like gestational diabetes, maternal obesity, and even smoking can steer your child toward faster BMI gains (ECHO Program).
Want a study saying it louder? Nature’s latest dives into how more than half the genes tied to obesity show up in early life (Nature Obesity Genetics). That’s why conversations with your OB–gynecologist about weight management start so early—from vitamins to exercise. That umbrella of prenatal care lingers way into toddlerhood!
Why Toddler Growth Can Be a Secret Goldmine
Think of toddler growth as a movie preview. If the scenes are muddy—say, skyrocketing weight gain with no slowdown—uh-oh, that might predict the blockbuster that follows! Project Viva called this “early BMI rebound,” or a second growth surge after infancy (Project Viva Study, 2019). If that jump happens before age 4, childhood obesity risks climb faster than a kid treats a cookie jar.
Move Over, Diapers: Here’s What Really Matters
Ahead of bedtime stories and snack packs comes this truth: what happens between age 1 and 3 can be a secret compass for health later on. The LongITools 2025 study even found generational differences in BMI trends—it’s not just your kid being… unpredictable. Society’s habits shift, just like kids’ shoes (can’t go from tiny Asics to Crocs. Or maybe some can).
Why Childhood BMI Patterns Are BOTH a Problem and a Clue
When “Normal” Gets Tricky
Look, BMI has some value—it’s like a base_script. But alone? It’s incomplete. Think of it like relying on a car’s fuel gauge with no dash cam. Sure, you know how much gas you have, but what’s happening under the hood?
A kid with a “low stable” BMI might still have poor nutrition and low physical activity—red flags not shown on a chart. Meanwhile, that high-achieving ballet prodigy with dense muscle might masquerade as “overweight” just from muscle’s weightiness (remember, muscle and bone affect stats) (MedicineNet). So yeah, it’s messy.
The Good and the Hiccup
Ok, so it’s flawed—but here’s why it’s still worth paying attention to. CDC data shows consistent “high rising” patterns? They do link to blood pressure issues and type 2 diabetes later on (CDC BMI Categories). And get this: obese kids are more likely to suffer self-esteem dips early. “It felt like trying to figure out a puzzle without the right pieces until we met a nutritionist,” mom Lisa sighed.
Here’s the Highlight: Early “Early” Action Matters
Old belief: “Kids will outgrow it.” New data: 70–80% of teens with obesity become obese adults (Global Obesity Statistics, 2023). Meantime? PMC’s 2025 review found that kids with early BMI gains saw physical limitations by teens even before obesity kicked in (Childhood Health Review).
But again—don’t Instagram panic. Seeing a climb too early? Pause. Ask, “What could shift this?” rather than “Is my child doomed?” Stay dialed in. There’s hope even if they’re rising fast. Let’s look at how to tell when it’s time to step in. Warning: we’re not consultants here. Just your friendly, caffeine-fueled parents trying to help!
What Can Pre-Adolescent Health Reveal About BMI Trajectories?
If the BMI Pattern Ain’t Normal, Could Their Health Follow Suit?
Let’s fast forward—if puberty hits and your kids’ BMI is still scaling the 90th percentile chart, heart health might take a small, invisible hit. PMC research showed higher BP can show up (Childhood BMI & Blood Pressure, PMC). Meanwhile, if the BMI curve tilts downward, like a creek drying in the desert, deficiencies (iron, vitamin D) might hide there instead.
Invisible Risks: The Ones You Can’t See (Yet)
“My son’s BMI was at 70th percentile, but he started getting angry tantrums—ahead of any weight gain,” shared a teacher in our Facebook parents’ group. Was this a fluke? Nope. PMC data from 2023 tied higher BMI to behavioral challenges like anxiety and emotional issues (Behavior, BMI, and Kids, 2023). So, it’s not just bodies that change; mindsets do, too.
Little tweak here—don’t slip into fear. These patterns are markers, not verdicts. The research reminds us: trends matter way more than one glucose pill. Monitor with calm, but act with purpose. How? Read on.
Moving Forward: Understanding the Full Picture of BMI in Kids
So… What Should You Actually Do With This Info?
Let’s get real. You don’t want jargon—you want answers that stick. Here’s a cheat sheet:
- Track trends, not single numbers. Like how jazz isn’t just one note played over and over.
- Nutrition + sleep = everything. Two things studio-schooled kids don’t get enough of.
- Talk to your pediatrician about trajectory modeling. Fancy techniques to spot red flags early. (perfect for the under-5 set).
Habits That Outgrow the BMI Chart
In 2025, the game isn’t “fix your child’s BMI.” It’s about creating lifestyle anchors they’ll carry with them—like family traditions of veggies after school or dancing while vacuuming (we know, those TikTok life hacks). Contagion Live’s study even found that antibiotics (a toddler staple) have negligible effects on BMI milestones (Antibiotic Impact). So no, diagnosing weight issues at the grocery store shelf isn’t fair.
Real Risks to Watch For
Sometimes, BMI is a red flag. Case in point: 2025’s LongITools study says kids with unseen-at-first “off-range” patterns ended up facing double the obesity risks. And remember, that 95th percentile metric isn’t just for show—it’s linked to Type 2 diabetes, sleep disruptions, and connected minds. StatPearls hammered it home: childhood obesity maps to early mortality and chronic diseases (NationObesity Research).
And yet… not every high BMI kid will need to carry a badge for disease trackers. Some kids just boil over the curve before leveling out. The key? How consistent the climb is. One 90th percentile point? Not a drama. A 90th percentile slide over 3 years? Now you’re talking.
Scoreboard: Healthy Trends vs. Hidden Pitfalls
| Healthy Trends | Pitfalls Hiding Behind BMI |
|---|---|
| Maintained within percentile range | Exposed to poor diet/activity early on |
| Teaches self-care habits early | Body fat shifted to visceral organs |
| Promotes physical and emotional resilience | High BMI increases pre-adolescent bullying |
How Clinicians Predict… (And Track) BMI Patterns Today
It’s Not ‘Just Weighing Kids In’—It’s Smarter Than That
Pediatricians aren’t just checking weight. They’re mapping growth math—no, not algebra. Trajectory modeling, to be precise! Like a fancy GPS for growth, this system uses data from over their first five years to hazard a guess about what’s coming next. Cool, huh? Nature’s team discovered genetic markers can intensify these calculations (Genetic Obesity Study, 2021).
Finding the Sweet Spot for Intervention
Would you catch a leak with sandbags fifteen minutes after it starts? Same concept. The sharpest window for parents (and clinicians) is before age 3.5. A self-reported weight study from MedicineNet warned that relying on my cousin’s cousin’s cousin’s memory of height at age 5 is an iffy strategy (BMI and Misreporting).
Pro tip: “If I notice fast slopes more than 2 vertical lines before age 4,” one pediatric nurse said, “I usually nudge parents toward lifestyle tweaks—not shame-and-blame.” That kind of practice lines up with Mayo Clinic advice (Mayo Clinic Childhood Obesity).
Making Pre-Adolescent Health a Priority
Can Zeros on a Scale Define Your Child’s Future?
Let’s think deeper. While your pre-teen line dances toward the 10-year mark, flat habits crash harder than a video game character: poor exercise, processed snacks, sugar over hydration. Contagion Live hits this point—it’s not about getting them into Olympic shape, but establishing a rhythm of resilience early (Antibiotic Study).
Here’s the Food for Thought: It’s Never Too Early—or Too Late
Remember: Healthy habits aren’t a diet or a race to losing weight. They’re lighthearted chore patterns, like grinding a smoothie instead of the classic candy jar. Even if your child is already on an atypical BMI track, small course corrects can bring powerful benefits.
One last tieback: the power of Nutrition Scores. The 2025 ECHO analysis showed kids with BMI reduction interventions before age 5 had dramatically improved chances of avoiding obesity throughout adolescence (JAMA ECHO Study).
A Few Final Thoughts: Your Child’s BMI Pattern Is Their Unique Path
In a world where algorithms see kids like rows in a spreadsheet, let’s remind ourselves—it’s not all numbers.
Your child’s body (and BMI) has its own story to tell. Maybe they’ll grow up mostly lean-stable like their dad. Or maybe they’ll take their lanky sister’s developmental road. Either way, don’t hand your child a label. Hand them tools. Their patterns can shift. Trajectories can learn to reroute. It’s about asking yourself:
“Are we moving in a direction that gives them strength—or distraction?”
Soak it in. Low stable or high climbing—there’s room to breathe. Room to grow. And more than anything? Trust your gut. You know your kid better than a spreadsheet. After all… you’re the ones walking through the bedtime tantrums and missing child tags. This is your terrain.
Want to sit with other worried yet curious parents on this topic? Drop a “Let’s unpack” below. If you’ve navigated your child’s tricky BMI dynamic, share your story not from fear—but from faith in the process. You’ve got this.























Leave a Reply
You must be logged in to post a comment.