You Ever Wonder What Makes a Child’s Heart So Special… and So Fragile?
You ever hold a little kid’s hand and feel their heartbeat? Like, really feel it? Nervous to mess up, right? But here’s the thing: those tiny ticker sounds are powered by valves about the size of a pushpin. And if something goes squeaky in there—like a bouncy castle with a slow leak—that “minor” issue?
Yeah, it can basically shut down the whole system.
We’re not just talking about kids needing rest. Ignoring hints of pediatric heart valve trouble can spiral fast. Seizures, trouble feeding, blue lips… Symptoms that might seem like toddler tantrums could actually mean surgery is on the table. Not “one day maybe,” but nine months old maybe.
Imagine sitting in a hospital bed with your child post-op, staring at a catheter taped under their chin, and trying not to cry because their nurse just patted your shoulder and said, “This is more common than you think.” Well, it is—and that’s why understanding this isn’t just academic.
Okay, But Let’s Get Real: What Makes This Whole “Valve” Thing So Tricky?
Alright, before we geek out on replacement heart valves (I promise it gets interesting), let’s break down why these weeny valves even matter. They act like tiny traffic cops inside the heart, directing blood flow so sticky oxygenated blood zooms through the right doors—and doesn’t reverse like a clown car at rush hour. When one goes funky, that combo of congenital heart defects and valve malfunction hits extra hard. Why?
- Their small size = Extra precision during surgery.
- Growing bodies = Replacements that might wear out in 3-5 years.
- Families’ emotional rollercoaster = “Why them?” plus logistics of clinic visits and meds forever.
So What Even Is Preclinical Testing?
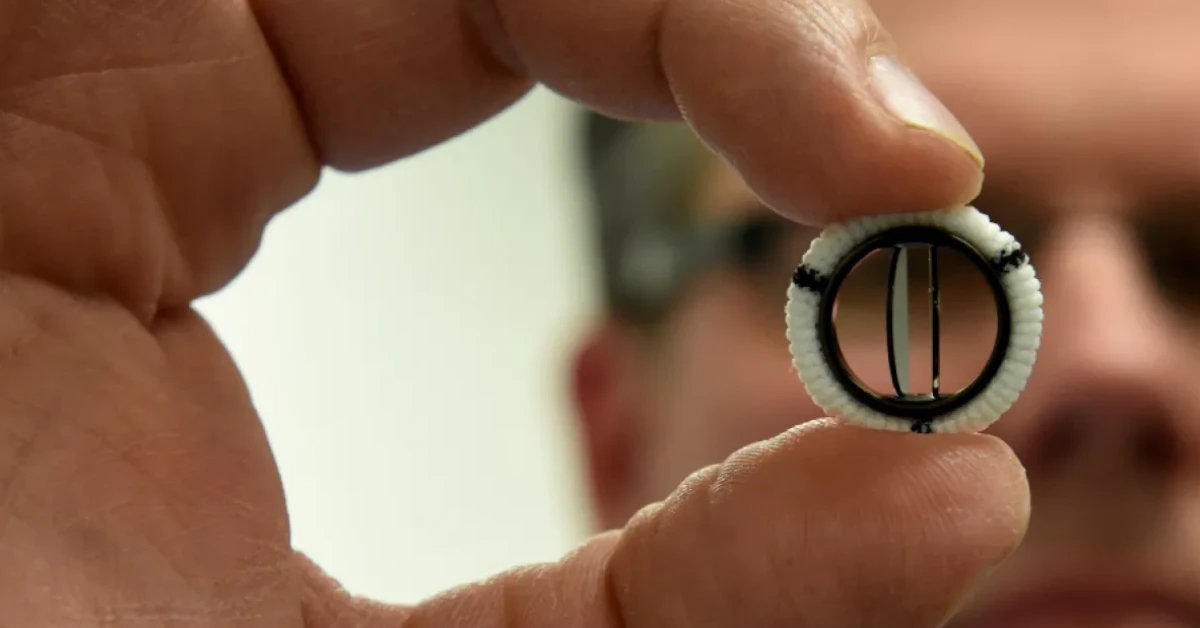
Think of it like sonic testing a new rollercoaster design before letting kids on it. UC Irvine researchers recently tested their new replacement heart valve in labs (not humans yet—patience, we’ll get there!). They mimicked toddler heartbeats and pressures with a squishy jellylike tube instead of veins yep, pretty wild. A study out of the Journal of the American Heart Association showed promising movement toward a valve that adjusts with a growing heart.
We’ll unpack what that means for real-life toddler diaper struggles in a bit. First, let’s talk valves. No jargon here—just practical deets.
Let’s Chat Replacements: Mechanical vs. Biological (and the New Wild Card)
If your child is staring down a heart valve replacement, you’ll hear terms like “mechanical” and “biological” GET ready. Both work, but choosing one feels like picking a backpack—depends on where the journey takes you.
Biological Valves: The “Whoa, That’s Cool!” Option
These are made from cow, pig, or human donor tissue (bovine is most common). Think of them like “baby steps”: older, tested, and soft, just like a plush bear. But they usually need replacing after 10-15 years. Right, but this also means another surgery when your kid becomes a rollerblading, parkour-loving 12-year-old. Yeah, that’s not hypothetical—ask any pediatric cardiology team.
Mechanical Valves: The Durable Draftpick
These are the stainless steel crew—for decades. But catch: they sometimes rev up blood clot risks, requiring daily thinners. Not exactly ideal for, say, a kid slamming piles of books on a sibling (you know the drama). And let’s be honest: making a high-energy lil monkey swallow blood-thinner pills? Tears and tiaras involved.
Comparison Table: Mechanical vs. Biological Valves
| Aspect | Mechanical Valve | Biological Valve |
|---|---|---|
| Durability | Decades+ | ~10-15 years |
| Anticoagulants Required? | Yep | Usually not |
| Growth compatibility | Struggles here. | Older options shrink over time. (Newer ones might fix this… stay tuned.) |
And Then There’s That UC Irvine Study… Holy Stretch Goals!
Their test-tube valve—published in the Journal of the American Heart Association—stretches and stretches like hot glue pulled from a craft stick. Not just “we hope it works,” but structurally scored high against pressure-testing models. Could this end the dreaded double-op for kids? Researchers aren’t cheering yet—but they’re walking back preclinical labs with cautious smiles on.
The Real Talk About “Child Cardiac Surgery” (Because Yes, It’s Heavy)
Heart surgery for a kid? Nobody signs up for that. But if their valve’s built like a Jamón Iberico sandwich inside their body, deciding to totally open the chest is like swapping out a tire on a moving car—you want the pit crew to be spot on. Teams at pediatric cardiology centers? Yeah, they’ve done cerebral palsy apraxia care, neonatal transplants, you name it. Most of them have more reminders in their Google Calendar than extended family holidays.
Coping Post-Surgery: The Messy Middle
Let me tell you about Marisa. Her son James had valve surgery at 18 months. For months, he’d wake up sprinting unless held. She compared it to trying to sit a kangaroo down with a bribe of goldfish crackers. But here’s the secret sauce: prepping you for what’s next. That’s the real fight. Physical therapy can feel like a second career, but folks pull through—like James, giggling at his preschool’s bubble machine like nothing.
What Do Surgeons Really Prioritize?
A pediatric cardio surgeon once told me, “Imagine fitting a grand piano into a midget car.” Yeah—that’s the actual quote. They’re not just fixing parts but calculating growth and blood volume. If a valve feels too bulky, it might snag on part of their anatomy that’s still irregular like a gravel patch in a smooth road.
Testing, 1-2-3: Why “Heart Valve Testing” Isn’t Overkill
Sometimes this process feels like airport security for Kool-Aid—“we need to check everything today.” But testing matters. Like… matters. A toddler’s valve has to survive spring-loaded growth spurts, von Willebrand disease if it’s diagnosed with other congenital heart defects, and heartbeats maxing out at 150BPM during naptime refusal.
How Do They Even Measure All This?
Say hi to echocardiograms! Yep: medical jargon for “put jelly on the baby’s chest, press a sensor against their sternum like a game of now-you-hear-it, now-you-don’t.” The image? It’s like watching a jellyfish dance in slow motion—but that dance keeps your kid alive.
Other common indicators tested:
- The “heartbeat ballet” (arrhythmias)
- Whole-body oxygenation
- Valve motion on 3D scanners (which really do look like something from Meow Wolf’s gear,)
If This New Valve Shines, What’s Next? (Spoiler: Less Shopping Has to Go Through It)
The “How Close are You, Really?” Reality
So UC Irvine’s heart valve work looks hot in the lab—but does that mean we’re rushing to clinics? The short answer: Not quite. Think of preclinical testing like the promenade before a plunge into the deep end. “Proof of concept” means the design works, but real-kid trials? That’s years ahead still. And no one wants “valve in a kid” being that next TikTrend challenge.
Still… imagine fewer surgeries. Like, maybe your kid gets one op at age two instead of two or three through elementary school. For working parents pacing the waiting rooms, that’s everything.
What If It Turns Out… a Valve Could Grow?
Here’s my leap: if this baby-heart jelly-tube tech evolves, future toddlers might wear a heart valve that “learns” their rhythm the way you learn your child’s favorite nighttime lullaby over years, it just adapts. Cite what you will—if pediatric cardiology’s version of artificial jellyfish hearts rolls out, we’ll all be Googling so much. But until then: labs are baking… and we wait.
Big Kids, Big Decisions: Balancing Risks for the Long Run
Wait, So How Do You Evaluate “Is It Worth It?”
Easy answer: No one can tell you. Real answer? Let’s map risks against quality of life. If your kid’s born with a mitral valve that leaks like cheap caulking, and they haven’t hit speech therapy? Maybe valve surgery frees them up to babble instead of gasp.
Risk vs. Growth: Thinking It Through
| Scenario | Risk Consideration | Quality of Life Gains |
|---|---|---|
| Age 1: | Choosing biological valve = re-op at 6, 10, 15 | They eat peas and run! |
| Age 12: | Mechanical might suit (fewer ops) | No trauma waiting for second valve |
So, What Else Should You Know? (Because Obsessive Google-Stalking is Real)
You’re not alone—like, not even. Researchers, families, and their sweat-soaked shirtsleeves are working on kid hearts daily. For more details check the American Heart Association resources, but in short: keep listening to your child’s body, ask a ton of questions, and explain to younger siblings what’s going on. Love notes stuck on the ICU fridge help.
You’ve just plowed through intense deets—give yourself a hug, alright? Grab a latte and maybe text a support group member or two. Because progress—slow or sprint-level—is only driven by those who care year-round, not once their app alerts push them a reminder.
Still wondering about your child’s congenital heart defects? Don’t hesitate to talk with a specialist early. On the flip side, share this cover-all with a parent who might nod and say, “Ohhh, now I get it!”





















Leave a Reply
You must be logged in to post a comment.