Hi there! Let me cut straight to the chase. If you’re a parent, teacher, or school staff, here’s what you need to know: Neurological emergencies like seizures, trauma injuries from recess mishaps, and substance abuse or mental health crises are the top three reasons schools call EMS. Yeah, that’s a mouthful—but stick with me. I’ll walk you through how to spot these emergencies, what to do when they strike, and why every school should have a plan (spoiler: it’s not just for show).
Neurological Emergencies
Seizures: When Training Meets Reality
If you’ve ever seen a child freeze mid-sentence, their eyes staring blankly, or maybe drop like a stone during gym class… you know the terror. Seizures aren’t rare in schools. A study from Pediatrics journal shows up to 25% of school-aged kids (5–19 years) could face a neurological emergency. Imagine Sandra Moritz, a swim instructor in Wisconsin, watching her 4-year-old students splash around. Suddenly, one of them clutching their chest—turns out, it was a seizure, not drowning. Sandra acted fast, but not all schools have someone that prepared.
Seizures can stem from epilepsy, head injuries, or even stress (teens, am I right?). The key isn’t panicking—it’s knowing the steps. TN.gov’s guidelines recommend:
- Stay calm but immediate. Move furniture, cushion their head.
- Time the seizure with a watch—or even your phone (yes, even teachers get jittery).
- DO NOT hold the person down or stick fingers in their mouth (a hard no).
- Call 911 if it lasts more than 5 minutes, or if they’re in obvious pain post-episode.
Here’s the kicker: Neurological emergencies aren’t just rollover crises. Symptoms can mimic other issues—a child fainting versus one having a heart attack, or even a stroke. Weird, right? UF Health’s breakdown on 6–12-year-old development sheds light on how brain growth can affect what conditions pop up during school hours.
So How Common Are These Seizures?
The stats? Yeah, the stats are real. According to AAP’s data, schools across the country report seizures constantly. Like… beeping headset emergencies. Ten to 25% of all school-based injuries or episodes are tied to neurological emergencies. That’s like two kids per classroom having a moment kids their age shouldn’t have to deal with. Hmm.
Psychiatric Crises
Substance Abuse: The Hidden Threat
Now let’s tackle the elephant in the classroom—substance abuse. Yeah, schools deal with it more than we’d like to admit. It’s not just high schools, either; sixth graders experimenting, teens using vapes, or kids acting erratic after snorting a vape cartridge. A study tracked in PubMed (2022) saw a spike in these emergencies, and schools are stretched thin.
Picture this: You walk into a locker room where a kid slumped against the wall, unresponsive. Is it a panic attack? A depressive episode? Or could it be an overdose? The American Heart Association says kids as young as 4 can memorize 911 protocols, but teens need more nuance.
Substance Abuse vs. Panic Attack: Spotting the Difference
| Overdose | Panic Attack |
|---|---|
| Slow or irregular breathing | Rapid breathing, gasping |
| Pale, clammy skin | Flushed, hot sweat |
| Mixed-up sentences, drooping eyelids | Clarity (for the most part), yellowness around eyes |
Looks complicated? Well, here’s the good news. With the right training, even a substitute teacher can buy time until EMS arrives. Red Cross-style first aid in swim lessons, like Sandra’s program, teaches early responders to stay cool under pressure. Why start early? Because a dry emergency is practice. A wet one is real.
Mental Health: Not Just “Whining”
Teens collapse in math class. Sometimes it’s flu season. Other times? Pure panic. The line between a mental health crisis and a substance-related incident gets blurry fast—for example, a student shark-biting their lip while hyperventilating could signal an anxiety attack, but the same symptoms might point to fentanyl signs if you catch slippage. How to navigate? Don’t guess. Check basics: pupils, breathing sound, and any items nearby. If meds or paraphernalia pop up, yell EMS—in some cases, a hospital may be the safest place.
Trauma Injuries
Playground Perils: Why Even the Most Careful Can Trip
Remember when everyone thought bruises were “just part of being a kid”? You’re not wrong. But let’s face it—broken bones & concussions ain’t okay. The AAP estimates up to 25% of all childhood injuries—yikes!—occur during school hours. Falls while climbing, helmets not on, or that soccer game where Dave tried a slide tackle and his knee didn’t survive. Oh, the stories.
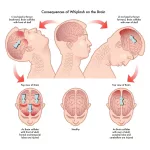
Kids are tiny daredevils. Elementary kids (5–10 years) seem immortal during recess until they’re not. The RICE method (Rest, Ice, Compression, Elevation) works for sprains—but what about concussions?
Concussion Red Flags: When “Shook, Not Stirred” Isn’t a Joke
Kids might laugh off a knock to the head, but concussions? They don’t care how tough they think they are. Check for:
- Silly spelling when asked to write (missed letters? Yeah, that’s a red zone).
- Double vision or nausea after a hit.
- Balance issues—can they stand on one foot? Seldom.
If unsure, better safe than sorry: call EMS. Better 15% false alarms than one missed critical case.
Emergency Planning
Without a Game Plan, Chaos Wins
I’ve seen schools try to wing it—even with staff swearing they “could handle anything.” Not cool. You need a real, not copy-pasted from a real-estate handbook, emergency plan. Washoe County has one that’s only 40 pages. Sure, sounds harsh until you realize each second lost fiddling through protocols could cost lives.
Who creates these plans? School nurses mainly, with AAP guidelines. Ever seen the annual Medical Response & Surge Exercise (MRSE)? It’s April 17, 2025, for starters. Perfect for updating your school’s plan. yeah, even a district cop needs the annual refresher. Here’s the thing: guidelines are useless unless you practice—one drill per semester, please.
CPR Training for Schools: Age Isn’t a Barrier
Ask yourself this: Can a kid in elementary grades learn CPR? CNN says, hell yes if taught right. The American Heart Association made updates too, including swimming drill instructors adding first aid to swim classes. And it works. Sandra Moritz isn’t just selling swim lessons; she’s teaching families how to help each other if the worst strikes—not just in pools.
2025 Deadlines You Don’t Want to Miss
Mark your calendar. In March, there’s a training drill in Minnesota (Doctor Invest?) where Sandra teaches. April’s MRSE event links school nurses to real-on-ground scenarios. And for schools looking to up their game, Red Cross’s Emergency Medical Response (EMR) 56-hour course runs from June to September. They’re tight spots to copy.
Connecting the Dots
Linking Water Safety and Seizure Risks
Now don’t leap here, but water safety goes hand in hand with seizure readiness. Sandra’s swim school isn’t just about dips —they simulate coughing and chocking incidents, yes, but they also ask parents to read up on health factors. Because a seizure in the deep end? Real messy. World Wide Swim School’s “Emergency Risk Ready” course adds training for environments you don’t always expect, like wet classrooms or overflowing labs. Creative, huh?
Catching the Big Wins for Staff & Students
Here’s the thing: training isn’t just for principals who need an autopsy later. Ed2Go’s 2025 sessions show teachers can relearn procedures quickly, and the cost? Yeah, less than losing a kid on a Monday morning. Even better: peer support systems. Have trained students who can spot withdrawal signs or a kid heading toward panic before they spiral. It works. My friend’s school did it—absences from anxiety dropped 30% after adding peer laughing hubs (okay, they called them “Chill Pods”).
The goal here isn’t to turn into ER nurses, but to know the basics. For me, it clicked when I myself blacked out briefly years ago; didn’t know how to help till someone else did. Could’ve been a locker sliding accident or something worse—who knew. That’s why we overcoach drills. You’re not a superhero. Just a prepared person. And that matters.
Final Thoughts
You knew this was coming—the hurry-up-and-train session. Let’s be honest: You can’t control every medical dilemma. But you can know what’s common and arm yourself. School emergencies aren’t rare. The March 12th session with Sandra Moritz? They’ve covered seizures, AED usage, and even water-based crises. Those are the small wins in huge security for tomorrow’s kids.
I leave you here: What’s your school doing well? What’s slipping? Ask around. Ladies and gents, if you’ve got a moment, throw a comment below. Let’s swap war stories, stumbles, and build something coaches can actually use. And if nothing else? Take one step. Sign up for June 11th’s Handling Medical Emergencies course. Diane the nurse actually said that after 14 years, she still learns something each time.
Stay sharp, stay human, and stay ready. Because sometimes all it takes is a mid-class collapse to test everything. Let’s pass.
























Leave a Reply
You must be logged in to post a comment.