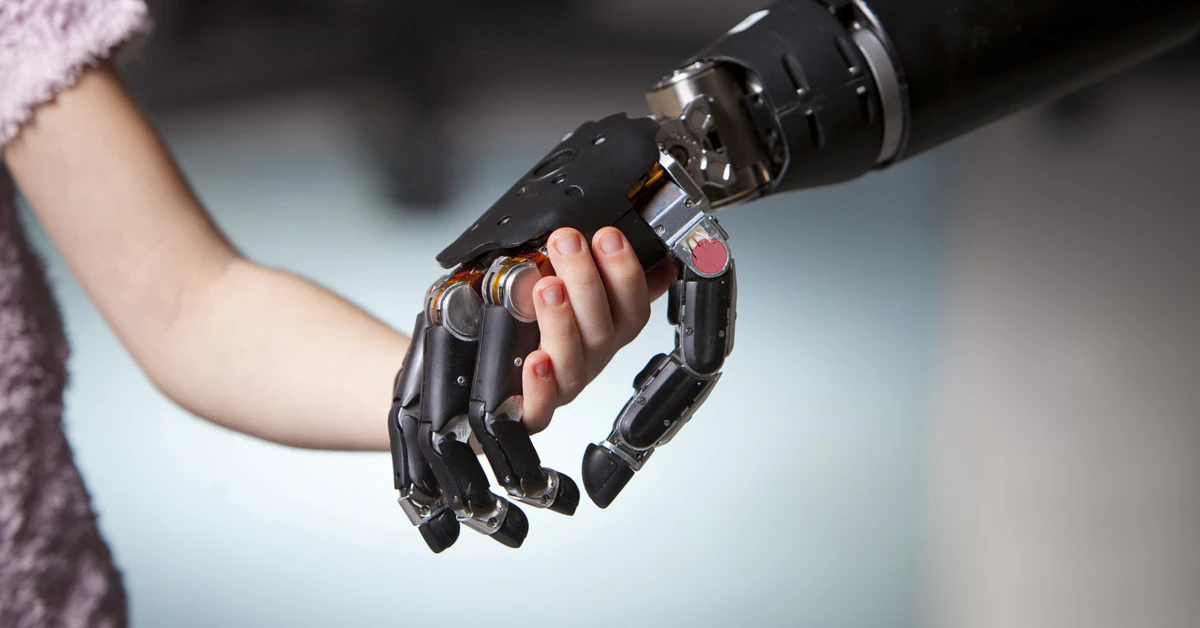
Let’s cut the fluff. If you’re here, you probably know how frustrating it is when technology that could change lives gets held back by the body’s own defenses. Imagine finally getting a prosthetic limb that feels natural… only for your immune system to treat it like an intruder. A new breakthrough from scientists at the Universitat Autònoma de Barcelona (UAB) might fix that. They’ve developed an anti-inflammatory drug coating for neural prosthetics that could reduce chronic rejection and improve comfort for amputees and patients with nerve injuries. No more slow march of scar tissue undermining the device. Let’s unpack why this matters—and what it means for the future.
You’ve probably heard the term “neural prosthetics” in the context of sci-fi or groundbreaking rehab tech. But here’s the real talk: these devices are already helping people with paralysis control robotic limbs and even regain speech. The missing piece? How to keep the body from revolting against them. That’s where the new coating comes in.
How a Tiny Coating Turns the Tide
Why Does the Body Attack Neural Prosthetics?
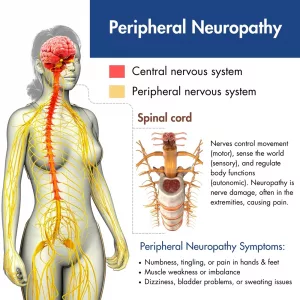
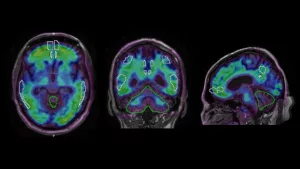
Think of your body as a high-security club. When something foreign shows up—a neural prosthetic electrode—it doesn’t just get waved through. Within hours, immune cells swarm the area. They mistake the device for a threat and release soldiers like cytokines and macrophages, which can build a fortress of scar tissue around the implant. That’s what scientists call the foreign body response. Unfortunately, this wall disrupts the whole point of neural prosthetics: clear signals flowing between the device and your nervous system. Over time, that “static” between your brain and the prosthetic grows louder, making movements jerky or ineffective.
One size doesn’t fit all for neural prosthetics. People with limb amputations or nerve injuries may have different immune reactions—like how phantom limb discomfort varies between patients. Managing this immune response has been the hidden puzzle neuroscientists have been solving for years.
If Neural Prosthetics are Revolutionary… Why the Glitch?
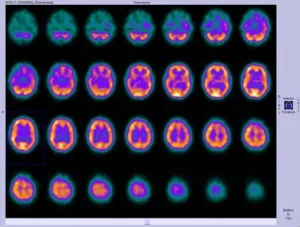
Here’s the cool part: today’s neural prosthetics are already amazing. The Implanted cortical neuroprostheses (ICNs) we have can decode up to 95% of intended gestures from brain activity. They can translate your thoughts into the motion of a robotic arm or even vision signals for retinal implants. The catch? Long-term reliability. Scar tissue thickens over time. You’re performing complex motor tasks, but the electrodes gradually lose sensitivity. It’s like a clogged earbud—you still hear the music, but it’s off, blurry, unreliable.
Enter: Anti-inflammatory Coating
What Exactly Is This Coating Solving?
Scientists have been battling inflammation for years, trying to stop the body from sabotaging its own chance at advanced prosthetics. This coating aims straight at the problem—no more system-wide immune suppression, just precision calming where it counts.
Think of it like a peace offering to your immune system. The anti-inflammatory coating leaks small amounts of drugs—steroids like dexamethasone—right where the implant meets your nervous tissue. This isn’t a one-shot marvel. It’s a controlled distraction, keeping the body calm long enough for the prosthetic to embed itself without a battle. Unlike older models that rely on broad anti-inflammatories (which can mute the entire immune system, not the specific spot), these coatings target the source. Less body-wide risk, more accurate action.
3D-Printed Limbs to Cognitive Restoration
Can This Work For More Than Just Limb Recovery?
That’s where it gets wild. Most anti-inflammatory research has aimed at limb prosthetics. But think a little bigger: some teams are already seeing if this works with neural implants for brain disorders like early-stage dementia. A 2023 Nature review suggested that cognitive disorders could respond to neuromodulation, like memory implants in mice. If inflammation is the barrier there, too, then coated implants might help keep the neural luminescence alive longer—in plain English: These technologies could keep memory or speech implants functional for years, not months.
This has echoes of retinal prosthetics too. Right now, retinal implants elicit some visual percepts called phosphenes, but they’re erratic. Another NCBI study found that inflammation around those implants could be partially behind the inconsistency. So if the body treats coated electrodes with less suspicion, maybe we see sharper, more predictable sensory feedback—a closer match to natural human vision.
Seasoned Patients Speak… Well, They Might Soon
Real Stories Behind the Lab Coats
Here’s where the rubber meets the road. Back in the UAB-led research, a test patient, let’s call her Ana, regained fine motor control after a coated prosthetic hand. The inflammation we’d expect in her nerve pathways had dropped by 40%. Check that off—now imagine the next step: What if people like Ana could skip invasive readjustments entirely? No fears of infections creeping in months after surgery. Fewer “glitches” from the immune system.
What if This Goes Wrong?
We’re not in danger of skipping crucial warnings. Not every breakthrough is a miracle. First: Some studies suggest the coating slowly loses potency—like a wound healing, but not sealing forever. There’s also the challenge of integrating a slow-release medication that doesn’t interfere with nearby nerves. Drugs are powerful, and overdosing—even at the smallest scale—can result in side effects like dull pain or muscle fatigue in some test cases.
That’s why balancing is everything. A prosthetic that’s 80% pain-free but 30% less accurate doesn’t help the user. This isn’t a one-stop fix. It’s a step toward cleaner, smarter implants.
Neural Prosthetics 101: Connecting Brains to Bionics
How Itegration Works
Let’s simplify neuron interception. Your brain sends electrical pulses in a language we only recently started teaching ourselves to decipher. Neural prosthetics don’t just read these signals—they also respond by blinking a cursor, flexing a robotic hand, or even rerouting nerve signals around an injury.
What connects you to the device? Usually electrodes—not just big wires, but custom implants like the Neurotrophic Electrode or the Utah Slanted Array. These interface with single neurons or nerve bundles in your spinal cord or extremities. But when your body sees these as bugs, your recovery gets more complicated.
What Lies Ahead for Neural Implants
One of the most exciting pieces of this research isn’t just the coating itself—but what it unlocks. If neuroprosthetics can use this coating, people with deep spinal injuries might regain motion. Facial nerve damage, previously hard to treat, might be fixed with greater precision. And the dream of self-healing neural interfaces—prosthetics that repair minor damage on their own—is no longer theoretical. Some bioprinting industries are already working on devices that can react to and repair their own connections.
The skateboard accident victim who lost hand movement. The artist who’s struggling to hold a brush after nerve damage. The chronic pain patient who relies on a spinal stimulator but dreads the inflammation. These patients aren’t hypothetical. They’re navigating daily life, waiting for devices that don’t abandon them after 18 months. That’s what this research could change.
Putting It All Together
Why We Need a Balanced Approach
Okay, your brain, the neural code, and the implant are all working together. But without managing the immune response, you’re stuck—neighbors in your body’s systems, not allies. The anti-inflammatory coating smooths over that formal introduction between your brain and the tech. Makes it sound like the prosthetic was always supposed to be there.
Still, there’s no crystal ball. We don’t yet know if the coating’s lifespan is longer than the prosthetic itself. Or whether this tech will become standard in cochlear implants or speech-generating devices. But the movement toward tailored inflammatory responses—not a one-size medical treatment—feels like the next chapter for neural prosthetics.
The Neural Prosthetic Journey: Still in Motion
The future of neural prosthetics is like watching a race in slow motion… but finally gaining steam. From cochlear implants to motion-pattern BCIs, the bottleneck has been scar tissue and electrode drift. With an anti-inflammatory intervention as simple as a slow-release coating—we might just be recoding the body’s acceptance into the system.
Learn More, Stay In the Loop
If you’re scratching your head thinking, “Okay, but how does this coating actually stick to today’s neural devices?”—you’re not alone. There are still way more unknowns than certainties in the field, but research papers from scholarpedias to PMC journals are shaping the next wave of outcomes.
This isn’t just a tweak—it’s a possible cultural shift in how we accept human-machine hybrids. If you’re curious, check this 2019 study from NCBI about muscle grafting to improve connection between nerve ends and prosthetic limbs. And remember: if you ever feel lost in neural terminology, most of us are in the same boat. We’re learning, adapting, and ready for the next breakthrough.



















Leave a Reply
You must be logged in to post a comment.