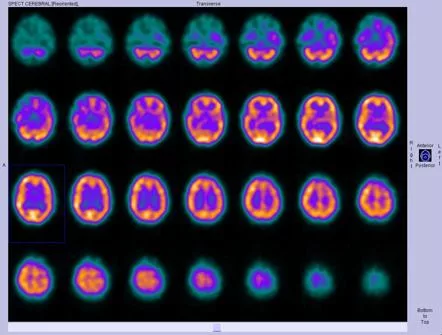
Most people don’t realize that a tiny amount of radioactive material can actually light up the brain and show us what’s really happening inside. In just a couple of sentences you’ll learn what radiotracer brain imaging is, why it matters, and how it can help you or a loved one navigate a confusing medical journey. Grab a coffee, settle in, and let’s explore this fascinating technology together.
How Tracers Reach
What Is a Radiotracer?
A radiotracer is a specially designed molecule that carries a radioactive atom—think of it as a tiny lantern that glows when it meets the right chemical environment. The most common lanterns for brain scans are fluorine‑18 (18F) and carbon‑11 (11C). When the tracer binds to a target such as glucose, dopamine receptors, or inflammatory proteins, a PET or SPECT scanner detects the emitted photons and turns them into colorful images.
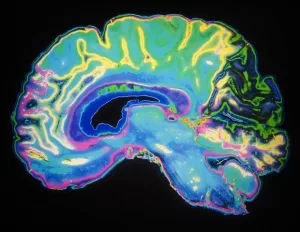
Crossing the Blood‑Brain Barrier
The brain protects itself with the blood‑brain barrier (BBB), a selective wall that blocks most substances. For a tracer to be useful it must be lipophilic enough to slip through yet specific enough to stay attached to the target once inside. Researchers have spent decades tweaking chemical structures to achieve this balance. Pike 2009 explains that optimizing size, charge, and polarity is essential for crossing the BBB without being kicked out by efflux pumps.
Surviving Metabolism
Once the tracer reaches the brain it must survive the body’s metabolic machinery long enough to be imaged. If it degrades too quickly, the signal becomes blurry and unreliable. That’s why many tracers are built on stable backbones—like the glucose analog 18F‑FDG—that resist breakdown while still interacting with the brain’s biochemistry.
PET vs. SPECT: A Quick Comparison
| Feature | PET | SPECT |
|---|---|---|
| Typical Isotope | 18F, 11C | 99mTc, 123I |
| Spatial Resolution | 3–5 mm | 8–10 mm |
| Radiation Dose | Lower (≈5 mSv for brain) | Higher (≈7 mSv for brain) |
| Common Uses | Metabolism, receptors, amyloid | Perfusion, inflammation (TSPO) |
What It Shows
Neuroinflammation
If you’ve ever wondered how doctors spot hidden inflammation in multiple sclerosis or traumatic brain injury, the answer is often a neuroinflammation PET scan. Tracers such as 11C‑PK11195 or the newer 18F‑DPA‑714 bind to the translocator protein (TSPO) that lights up on activated microglia—the brain’s immune cells. The resulting images reveal hotspots of inflammation that would be invisible on a regular MRI.
Glucose Metabolism (FDG‑PET)
18F‑FDG is the workhorse of brain PET. It mimics glucose, the brain’s primary fuel, and its uptake mirrors neuronal activity. Reduced FDG uptake in the posterior cingulate and temporoparietal cortex, for example, is a classic sign of Alzheimer’s disease, while focal hyper‑metabolism can hint at seizures.
Dopamine System & Movement Disorders
For Parkinson’s or other movement disorders, doctors often ask for 18F‑FDOPA or 11C‑raclopride scans. These tracers map dopamine synthesis or receptor availability, helping to differentiate Parkinson’s disease from other tremor‑causing conditions. Kilbourn 2021 provides a thorough review of how these agents have evolved over the past four decades.
Amyloid & Tau Imaging
When early detection of Alzheimer’s becomes crucial, amyloid tracers (18F‑Florbetapir, 18F‑Florbetaben) and tau tracers (18F‑Flortaucipir) step in. They bind to the protein plaques and tangles that define the disease, often years before symptoms appear.
Seizure Focus Localization
Patients with refractory epilepsy may undergo an interictal FDG‑PET or a SPECT with 99mTc‑HMPAO. Areas of reduced metabolism or perfusion point to the seizure focus, guiding surgeons toward a targeted resection.
The Imaging Workflow
Patient Preparation
Before the tracer is injected, you’ll likely be asked to fast for 4–6 hours (especially for FDG) and avoid caffeine or strenuous exercise. Medications that affect the brain’s chemistry—like anti‑seizure drugs—may need to be paused, but only under your doctor’s guidance.
Tracer Production & Quality Control
Most large hospitals have an on‑site cyclotron that creates the short‑lived isotopes. Once the molecule is labeled, it undergoes rigorous quality checks: radiochemical purity > 95 %, sterility, and pH within a physiological range. This ensures the tracer is safe and will give a clear image.
Injection and Uptake
After a quick IV line is placed, the tracer is injected, and you’ll wait for it to distribute. Uptake times differ: FDG needs about 30 minutes, while TSPO tracers often wait 60 minutes. During this period you’ll sit in a quiet, dim room—no need to move, just breathe calmly.
Scanning the Brain
Modern total‑body PET scanners like the EXPLORER can capture the whole brain (and even the rest of the body) in a single, rapid sweep, dramatically reducing radiation dose. The scanner rotates around you, detecting the emitted photons and feeding them to a computer that reconstructs a 3‑D image.
Reconstruction & Quantification
Raw data are turned into visual images using algorithms that correct for scatter, attenuation, and motion. The resulting numbers—Standardized Uptake Values (SUVs) or binding potentials—let clinicians compare the tracer’s concentration across regions and to normal reference values.
Interpretation & Reporting
Radiologists and nuclear medicine physicians follow a structured reporting template: clinical question, visual findings, quantitative metrics, and a concise impression. A clear report helps neurologists decide on treatment plans or further testing.
Safety & Radiation Dose
Radiation from a typical brain PET is about 5 mSv—roughly the same as a CT scan of the chest. For most adults the risk is negligible compared with the diagnostic benefit. Pregnant patients are usually excluded unless the information is absolutely essential for the mother’s health.
Benefits vs. Risks
Key Benefits
- Molecular specificity: See chemistry, not just anatomy.
- Early detection: Spot disease before structural changes appear.
- Therapy monitoring: Watch how a drug engages its target in real time.
- Research value: Accelerates drug development and clinical trials.
Potential Risks
- Radiation exposure—generally low, but cumulative dose matters.
- Allergic reaction to the tracer (rare, usually mild).
- False positives/negatives if the image is read without clinical context.
Patient‑Centred Counseling
When your doctor discusses a scan, ask about the purpose, the radiation dose, and what the results could change in your care. Knowing the “why” turns anxiety into empowerment.
Regulatory & Insurance Landscape
Most PET tracers are FDA‑approved or have “research use only” status. Insurance coverage varies; a pre‑authorization letter citing clinical guidelines often smooths the process.
Future Directions
Next‑Gen Inflammation Tracers
Emerging fluorine‑18 TSPO ligands promise higher signal‑to‑noise ratios and easier production. Studies on molecular imaging inflammation suggest they could become the new standard for tracking neuroinflammation across many disorders.
Hybrid PET/MRI Systems
Combining PET’s metabolic detail with MRI’s exquisite anatomy provides a “one‑stop shop” for neurologists. You get high‑resolution structural maps alongside tracer distribution, all without extra radiation.
Total‑Body PET (EXPLORER)
The EXPLORER scanner can image the entire body in a single breath‑hold, cutting scan time and dose dramatically. This breakthrough is already reshaping oncology and shows promise for brain research, especially for longitudinal studies where repeated scans are needed.
Theranostics: Diagnosis + Treatment
Imagine a tracer that not only shows you where disease lives but also delivers a therapeutic payload. Researchers are pairing diagnostic isotopes (like 18F) with therapeutic ones (like 177Lu) on the same molecular scaffold—a true “theranostic” approach.
AI‑Driven Quantification
Deep‑learning algorithms can now auto‑segment brain regions and extract SUVs in seconds, reducing observer variability. While still under validation, AI promises faster, more consistent reports.
Conclusion
From the moment a nanogram of radio‑labeled molecule is injected, radiotracer brain imaging begins a remarkable journey across the blood‑brain barrier, lighting up metabolism, inflammation, or receptor activity that would otherwise stay hidden. The technology blends cutting‑edge chemistry, high‑resolution scanners, and skilled physicians to give us a window into the living brain—one that can diagnose, guide treatment, and even accelerate drug discovery.
Understanding both the benefits and the modest risks empowers you to make informed choices with confidence. Whether you’re a patient, a caregiver, or simply a curious mind, the ability to visualize the brain at the molecular level is a powerful tool in modern medicine.
If you want to dive deeper into specific tracers, explore our articles on PET tracer brain inflammation or learn more about how PET imaging brain inflammation can change lives. The science is evolving fast, and staying informed means staying ahead.



















Leave a Reply
You must be logged in to post a comment.