Living with hidradenitis suppurativa (HS) can feel like carrying a tiny, persistent fire under your skin. The throbbing, burning, or stabbing sensations often show up at the worst possible moments—during work, family time, or even when you’re trying to relax. The good news? You don’t have to accept that pain as “just part of life.” With the right mix of medications, simple at‑home tricks, lifestyle tweaks, and—when needed—professional procedures, you can tame the pain and reclaim your day‑to‑day comfort.
In the next few minutes, we’ll walk through the science behind HS pain, explore step‑by‑step treatment options, and help you build a personalized plan that balances relief with safety. Grab a cup of tea, settle in, and let’s demystify the path to hidradenitis pain relief together.
Understanding HS Pain
What makes HS painful?
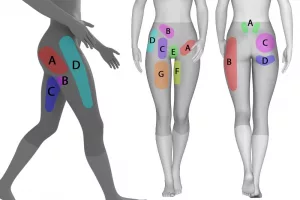
HS lesions are more than just irritated skin. They’re inflamed plugs in the hair follicles that can rupture, spill inflammatory material, and irritate nearby nerves. This creates two main pain types:
- Nociceptive pain – an aching, gnawing sensation that comes from tissue damage. Think of it like the soreness after a bad sunburn.
- Neuropathic pain – a burning, electric “pins‑and‑needles” feeling that occurs when nerves themselves get messed up.
A patient guide notes that many people use words like “throbbing” for nociceptive pain and “burning” for neuropathic pain. Knowing which flavor you’re dealing with can steer you toward the most effective treatment.
Acute vs. chronic patterns
HS pain isn’t a one‑size‑fits‑all experience. During a flare, pain can spike sharply—often described as “sharp” or “stabbing.” Between flares, a low‑grade, constant discomfort may linger, especially if scar tissue or sinus tracts have formed. Both impact quality of life, but chronic pain tends to erode mood and sleep more insidiously.
Quick self‑assessment
Before you dive into any treatment, try this short checklist:
| Question | What to look for |
|---|---|
| Intensity (0‑10) | Are you above 4 on most days? |
| Type | Aching/gnawing vs. burning/shooting? |
| Timing | Only during flares or constant? |
| Triggers | Friction, sweat, stress, hormonal cycles? |
Jot down your answers—you’ll find them handy when you talk to your dermatologist or pain specialist.
First‑Line OTC Relief
Topical anesthetics
Lidocaine 2‑5 % gels, creams, or patches are a quick‑acting friend for open lesions. Apply a thin layer directly onto the sore area (no more than 5 g total), and you’ll often feel a soothing “numb” sensation within 10‑15 minutes. The 2021 JAAD algorithm recommends lidocaine as a frontline choice for acute flare pain.
Oral acetaminophen
If you’re looking for a gentle, liver‑friendly option (as long as you stay under 4 g per day), acetaminophen can dampen mild to moderate pain without the stomach irritation some NSAIDs bring. It’s especially useful when you have a sensitive gut or are on blood thinners.
Non‑steroidal anti‑inflammatory drugs (NSAIDs)
Ibuprofen 400‑600 mg every 6‑8 hours or naproxen 250‑500 mg twice daily tackles both inflammation and pain. Just remember to take them with food, and check with your doctor if you have a history of ulcers, kidney issues, or are on certain blood pressure meds.
OTC Pain‑Relief Kit (quick reference)
| Product | Typical Dose | When to Use |
|---|---|---|
| Lidocaine 5 % gel | Apply sparingly to lesion, max 5 g | Acute flare or before dressing change |
| Acetaminophen | 500‑1000 mg every 6 hr (≤4 g/d) | Mild‑moderate pain, any time |
| Ibuprofen | 400‑600 mg every 6‑8 hr (≤3 g/d) | Inflammatory pain, flare days |
Prescription Pain Options
Anti‑inflammatory & disease‑modifying meds
When OTCs don’t cut it, the next tier is prescription‑grade anti‑inflammatory agents. Oral antibiotics such as doxycycline (100 mg twice daily) have a dual role: they fight hidden bacteria and dampen the immune response, often shrinking nodules and easing pain over a few weeks.
Biologics—particularly adalimumab (Humira) and infliximab—target the TNF‑α pathway that fuels HS. A 2021 JAAD study showed that up to 80 % of patients on adalimumab experienced a ≥50 % reduction in pain scores after 12 weeks. These drugs don’t just quit the pain; they attack the root inflammation.
Opioid ladder for refractory pain
Opioids are like the “last‑resort fire extinguisher.” Follow the World Health Organization ladder:
- Tramadol (50‑100 mg q6‑8 h) – mild‑moderate breakthrough pain.
- Codeine or hydrocodone combos – step up if tramadol falls short.
- Stronger agents (morphine, oxycodone) – only for short bursts (≤5 days) and under strict monitoring.
Never use opioids as a daily blanket; they don’t treat the underlying lesions and can lead to dependence.
Neuropathic agents
If your pain feels “burning” or “electric,” you’re likely dealing with neuropathic pain. Gabapentin (starting at 300 mg at night, titrating up to 600 mg three times daily as tolerated) or pregabalin (75‑150 mg BID) can calm the over‑active nerves. Many patients also notice improvement in itch and mood because these meds have a modest antidepressant effect.
Prescription algorithm at a glance
Below is a simple flowchart you can sketch on a napkin:
- Start with OTC → if pain ≥ 5/10 for > 2 weeks → move to prescription NSAID or oral antibiotic.
- If pain stays high or becomes neuropathic → add gabapentin or switch to a biologic.
- Only when all else fails → short‑term opioid under strict supervision.
Procedural Pain Solutions
Surgical debridement & excision
When lesions become chronic tunnels (sinus tracts) or large abscesses, simply taking medication won’t soothe the pain. Deroofing (removing the top of a tunnel) or wide‑local excision excises the pain source. Post‑op pain is usually short‑lived and can be managed with the OTC regimen above.
Nerve block techniques
For especially stubborn pelvic or groin pain, dermatologists and pain specialists sometimes perform a superior hypogastric plexus block or a ganglion impar block. These injections temporarily “turn off” pain signals from the affected area. A 2024 case report described a 42‑year‑old woman who found lasting relief after a series of ganglion impar blocks, allowing her to taper off high‑dose opioids.
Laser & CO₂ resurfacing
Laser treatments can shrink tunnels and smooth scar tissue, indirectly reducing the pressure that leads to pain. They’re usually adjuncts to medical therapy, not stand‑alone cures.
Lifestyle Pain Modifications
Weight control and diet
Extra skin folds create friction, heat, and sweat—perfect breeding grounds for HS flares. Even a modest 5‑10 % weight loss can lower flare frequency and the intensity of pain, according to a 2023 patient‑guide analysis.
Skin‑care hygiene
Keep the affected zones clean, dry, and loosely dressed. Breathable fabrics (cotton, bamboo) reduce rubbing. After a shower, pat the skin gently—not rub—to avoid irritation.
Stress management
Stress ramps up inflammatory cytokines, which can flare HS and amplify pain. Simple practices—guided breathing, short walks, or a weekly yoga class—can lower the “central sensitization” that makes pain feel worse.
Gentle exercise
Low‑impact cardio (swimming, stationary cycling) improves circulation, helping the immune system clear inflammatory debris. Core‑strengthening moves also support the groin and axillary areas, decreasing friction.
Daily pain‑log template
| Date | Pain (0‑10) | Type | Triggers | Medications Used |
|---|---|---|---|---|
| 2025‑08‑01 | 6 | Aching | Hot shower | Lidocaine, ibuprofen |
| 2025‑08‑02 | 3 | Burning | Stress | Gabapentin |
Keeping a log helps you and your clinician see patterns and adjust treatment before pain spirals.
Build Your Pain Plan
Step‑by‑step worksheet
- Record baseline: Use the pain‑log for a week.
- Try OTC combo: Lidocaine + ibuprofen + acetaminophen for 5‑7 days.
- Re‑evaluate: If pain stays > 4/10, schedule a visit for prescription options.
- Discuss neuropathic meds: If burning dominates, ask about gabapentin.
- Consider biologics: If lesions are widespread and pain is chronic, a TNF‑α inhibitor may be the game‑changer.
- Escalate carefully: Opioids only for short breakthrough pain under specialist supervision.
- Layer in lifestyle: Weight, skin‑care, stress, and exercise throughout.
When to call a specialist
If you notice any of the following, it’s time to get a second opinion:
- Pain > 7/10 lasting more than a week despite OTC and prescription meds.
- Signs of infection (increased redness, fever, drainage).
- Difficulty sleeping or mood changes that interfere with daily life.
- Need for opioid doses that exceed the WHO “step‑3” guidelines.
Real‑world story
Sarah, a 38‑year‑old teacher, described her journey in a 2024 case report. After years of hopping between topical creams, antibiotics, and even a short course of oxycodone, she finally found relief when her dermatologist added adalimumab and a gabapentin taper, while a dietitian helped her lose 12 lb. Within three months, Sarah’s pain score dropped from 8/10 to 3/10, and she could finally stand for a full class without wincing.
Safety And Monitoring
Adverse‑effect checklists
Every medication comes with a “homework” list. Keep this handy:
- Acetaminophen: Watch liver enzymes if you exceed 3 g/day or drink alcohol heavily.
- NSAIDs: Check blood pressure, kidney function, and ulcer risk.
- Biologics: Screen for TB and hepatitis before starting; monitor for infections.
- Gabapentin: Note dizziness or mood changes; adjust dose if you feel “spacy.”
- Opioids: Track daily dosage, watch for constipation, and discuss taper plans early.
Follow‑up schedule
Typical monitoring cadence:
- Every 3 months while on a biologic (blood work, skin assessment).
- Monthly check‑ins for gabapentin or opioid adjustments.
- Quarterly review of lifestyle goals (weight, exercise, stress).
Building trust with your care team
Open, honest communication is the backbone of successful pain management. Bring your pain‑log, ask questions, and be clear about what side‑effects bother you. Remember: you’re a partner in the treatment plan, not just a passive patient.
Conclusion
Hidradenitis Suppurativa pain doesn’t have to dominate your life. By understanding the type of pain you’re dealing with, starting with smart OTC choices, progressing thoughtfully to prescription and procedural options, and weaving in lifestyle habits, you can craft a balanced, effective strategy. Keep a daily log, stay curious about how each treatment feels, and never shy away from asking for help when the pain climbs. You deserve relief—let’s take those first steps together.
What’s been your biggest hurdle in managing HS pain? Share your story in the comments, and if any part of this guide sparked an idea, let us know! We’re all in this together.






















Leave a Reply
You must be logged in to post a comment.