Public health reforms are the policy‑driven changes that shift our health system from a “treat‑first” mindset to a proactive, community‑centered approach that actually keeps people well. In simple terms, they’re the big‑picture moves that let us prevent disease, protect the most vulnerable, and stretch limited resources further.
Why does this matter right now? The Affordable Care Act (ACA) gave insurance to millions, but it also tucked in a suite of prevention‑focused provisions that are only beginning to show their full impact. Add to that the post‑COVID push for “Public Health 3.0,” and we’re at a crossroads where every reform can reshape lives—if we get it right.
Why Reforms Matter
What gaps did early 20th‑century medicine leave?
Imagine living in a city where clean water is a luxury, sewage leaks into the streets, and infant mortality rates hover above 150 deaths per 1,000 live births. That was the reality in many American towns before the turn of the last century. Early 20th century medicine focused on battling individual illnesses with limited tools—think rudimentary antibiotics and heroic doctors—while largely ignoring the environmental and social conditions that birthed those illnesses.
Case Study: Infant Mortality
When municipal water systems and sewer upgrades finally arrived, infant mortality plunged dramatically. A recent infant mortality study shows a 60 % drop in deaths among children under one year in cities that adopted modern sanitation between 1905 and 1925. The numbers speak for themselves:
| Year | Infant Mortality (per 1,000 live births) |
|---|---|
| 1905 (pre‑sanitation) | 158 |
| 1915 (mid‑implementation) | 108 |
| 1925 (post‑implementation) | 63 |
How does the physician‑decline affect public health?
Fast‑forward a century, and we face a different problem: fewer physicians entering the workforce, especially in rural and underserved areas. The ripple effect is stark—when primary‑care doctors vanish, community health departments lose crucial partners for vaccination drives, chronic‑disease screening, and health‑education campaigns.
According to a physician decline effects analysis, counties that lost more than 10 % of their primary‑care workforce between 2010 and 2020 saw a 7 % rise in preventable hospitalizations. It’s a reminder that public health can’t operate in a vacuum; it needs a steady flow of clinicians, nurses, and allied health workers to translate policy into practice.
Modern Milestones
The ACA’s hidden public‑health provisions
Most people think of the ACA as the “insurance bill.” Yet tucked inside are three powerful public‑health levers:
- Preventive services at no cost. Annual screenings, vaccinations, and counseling are covered without co‑pays, nudging millions toward early detection.
- Community health grants. Federal dollars now fund local coalitions that address obesity, tobacco use, and mental‑health stigma.
- Data‑sharing mandates. State health departments must report health outcomes to a national repository, creating a richer evidence base for future reforms.
Public Health 3.0 – a data‑driven upgrade
In 2024, Innovaccer outlined a six‑pillar framework for “Public Health 3.0.” The pillars—sustainable funding, interoperable technology, workforce diversification, equity focus, community partnership, and outcome measurement—form a roadmap for modernizing the system. Think of it as turning a squeaky, old bicycle into a sleek, electric bike that can zip through today’s complex health terrain.
Post‑COVID lessons: reboot or upgrade?
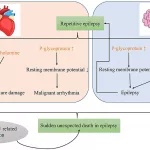
The pandemic exposed glaring weaknesses: an over‑reliance on hospital capacity metrics and a neglect of social determinants such as housing, food security, and employment. Harvard Public Health analysis argues that we must “de‑medicalize” public health—pulling the focus away from solely clinical solutions and toward whole‑society strategies.
Key Pillars of Effective Reform
Sustainable Funding
Public‑health programs die without steady cash flow. The 2024 White House budget proposes a flexible funding pool that blends federal, state, and private dollars, allowing health departments to pivot quickly in response to emerging threats (e.g., opioid spikes, climate‑related illnesses). A quick checklist for local leaders:
- Secure baseline financing for core services (vaccinations, surveillance).
- Allocate reserve funds for rapid response.
- Tie a portion of budgets to measurable health‑equity outcomes.
Data & Technology
Interoperable IT systems are the nervous system of modern public health. When data from hospitals, schools, and social services flow freely, officials can spot a rise in asthma attacks in a specific zip code and intervene with air‑quality measures before the problem snowballs.
Workforce Diversification
Public‑health teams need more than doctors. Social workers, epidemiologists, data scientists, community organizers, and even urban planners each bring a piece of the puzzle. The medical school closures impact report showed that regions with fewer medical schools struggled to attract non‑clinical public‑health talent, highlighting the need for intentional recruitment beyond the traditional pipeline.
Equity & Social Determinants
Health inequities aren’t random—they’re baked into policies that affect housing, education, and transportation. Scotland’s recent partnership between government and local authorities (see ScotPHN 2025 report) illustrates how aligning public‑health goals with affordable‑housing initiatives can cut chronic‑disease rates by 12 % in just three years.
Community‑Driven Decision‑Making
When citizens sit at the table, reforms stick. In California, a citizen advisory board helped redesign a “mobile health clinic” to better serve farmworkers, resulting in a 25 % increase in prenatal care visits. Listening to lived experience turns abstract policy into real‑world solutions.
Real‑World Impact
Sanitation Success in the Early 1900s
Back when urban water supplies were a luxury, cities that invested in clean water saw infant mortality plunge—proof that infrastructure is the foundation of health. This lesson still guides today’s push for clean‑air policies and safe drinking water in underserved neighborhoods.
Physician Shortages Ripple Out
Rural counties that lost primary‑care doctors after the 2010s experienced a surge in preventable ER visits. The physician decline effects study recommends tele‑health incentives and loan‑repayment programs to draw clinicians back into hard‑to‑staff areas.
Modern Wins: The Public Health 3.0 Blueprint
One mid‑size city applied the six‑pillar framework, investing in a unified data platform, hiring equity officers, and securing a blended‑funding model. Within two years, opioid‑related deaths fell 15 % and childhood vaccination rates rose to 96 %. The numbers illustrate how coordinated reform can deliver tangible health gains.
Common Pitfalls & How to Dodge Them
Over‑reliance on Hospital Metrics
Counting only hospital beds or ER visits ignores the upstream drivers of illness. Instead, blend clinical data with social‑determinant indicators like housing stability and food security.
Ignoring Community Voice
Top‑heavy decision‑making leads to “one‑size‑fits‑all” programs that miss local nuance. Always embed community advisory panels early in the planning process.
Under‑funding Prevention
Treat‑first budgets look cheaper on paper but cost more in the long run. Showing the ROI of preventative interventions (e.g., every $1 spent on vaccine outreach saves $3 in hospital costs) helps persuade policymakers to invest.
The Future of Public Health Reforms
Emerging Policy Proposals
Legislators are now debating a national public‑health fund that would lock in multi‑year financing, free from annual budget battles. If passed, it could guarantee stable resources for chronic‑disease prevention, climate‑health resilience, and mental‑health outreach.
Technology Road‑Map
Artificial intelligence could soon predict outbreak hotspots by analyzing sewage samples, social‑media trends, and climate data in real time. Coupled with equity dashboards, officials can allocate resources where they’re needed most—right when they’re needed.
Getting Involved
You don’t have to be a policymaker to influence reform. Join local health coalitions, attend town‑hall meetings, or simply share reliable information on social media. Every voice adds weight to the push for smarter, fairer health policies.
Public health reforms are more than legislation—they’re a collective promise to protect each other, especially the most vulnerable among us. By understanding the history, recognizing the current pillars, and watching for common traps, we can champion policies that truly make our communities safer and healthier.
What reforms have you seen in your neighborhood? If a local program made a difference in your life, share the story with friends—or start a conversation with your city council. Together, we can keep the momentum rolling.






















Leave a Reply
You must be logged in to post a comment.