Lumps and bumps in and around the vaginal area are common. They may be harmless or indicate an underlying issue that warrants medical attention.
If you’re noticing lumps, bumps, or areas of discolored skin near your genitals, you’re not alone.
This article outlines potential causes of changes in this region and explains when to consult a healthcare provider.
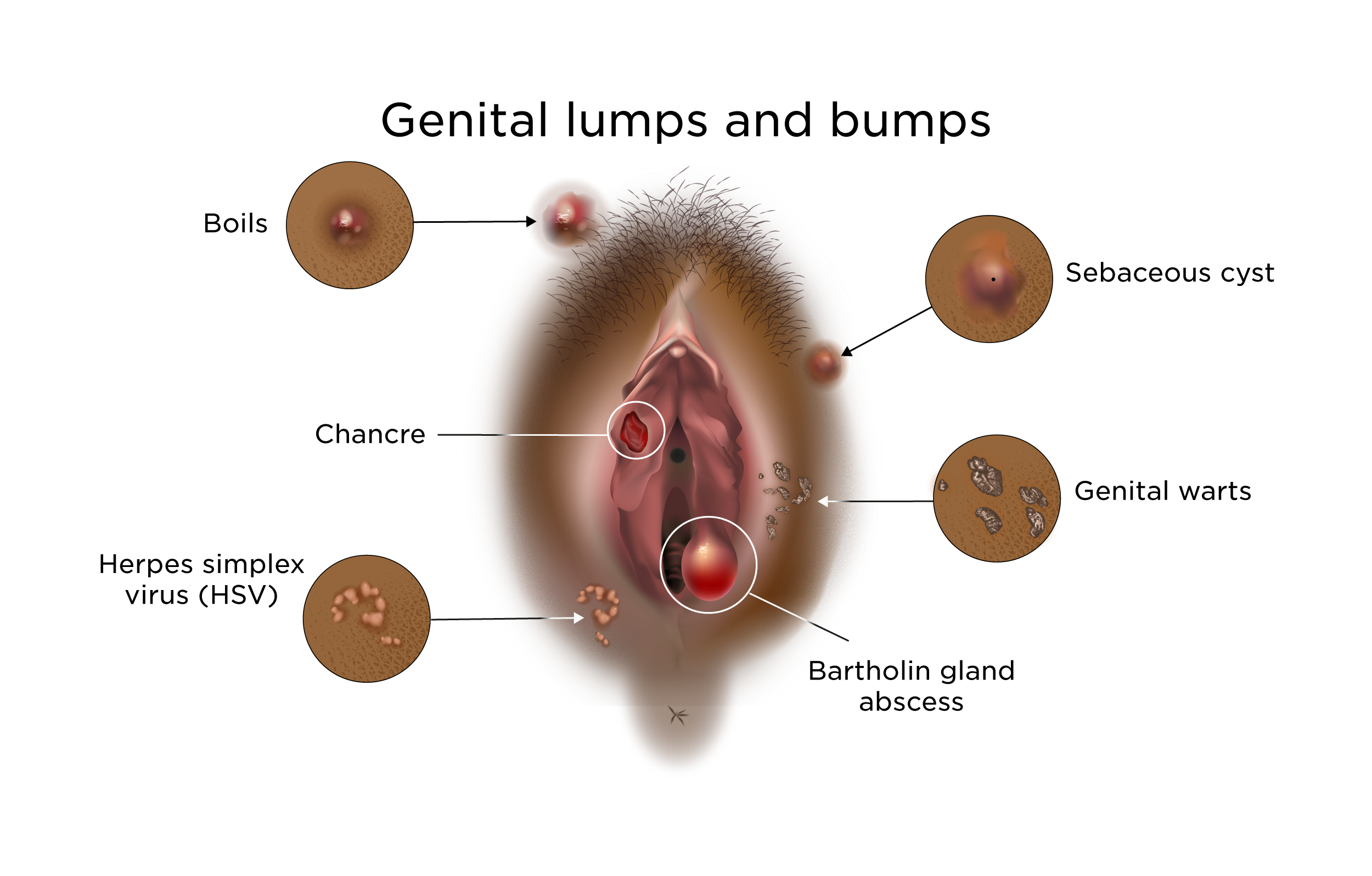
Causes of vaginal lumps and bumps
Below are 10 possible reasons for alterations to the skin of the vulva and vagina:
Vulvar cysts
The vulva contains numerous glands — for example, oil glands, Bartholin’s glands, and Skene’s glands. When these glands become blocked, a cyst can develop.
Cysts come in various sizes but often present as small, firm lumps. They usually aren’t painful unless they become infected.
Many cysts resolve without intervention. If infected, a clinician can drain the cyst, and antibiotics may be prescribed when infection is suspected.
Vaginal cysts
Several types of vaginal cysts exist. These are firm lumps along the vaginal wall and are commonly about the size of a pea or smaller.
Vaginal inclusion cysts are the most frequent form and may appear after childbirth or following trauma to the vagina.
Typically painless, vaginal cysts rarely present a problem unless they cause discomfort during intercourse. In some cases, they require drainage or surgical removal.
Fordyce spots
Fordyce spots (sebaceous glands) are tiny white or yellowish-white bumps located on the inner vulva. They can also occur on the lips and cheeks.
They often first show up during puberty and may increase in number with age.
Fordyce spots are benign and do not cause pain.
Varicosities
Varicosities are enlarged veins that may develop around the vulva. They can occur in up to 34% of people with pelvic varicose veins and in up to 22% of pregnant individuals.
These veins look like bluish raised lumps or rounded swollen veins around the labia. They may be painless, though sometimes they feel heavy, itch, or bleed.
Discomfort can occur during intercourse or after prolonged standing. A vascular specialist can provide treatment options.
During pregnancy, treatment is usually unnecessary, as varicosities commonly subside about six weeks after delivery. They can recur with future pregnancies, however.
Ingrown hair
Shaving, waxing, or plucking pubic hair raises the chance of ingrown hairs.
An ingrown hair can create a small, round bump that is sometimes painful or itchy. It may fill with pus, and the surrounding skin can become darker.
Most ingrown hairs clear up on their own. If inflammation or infection develops, see a doctor for evaluation and treatment.
Skin tags
Skin tags, or pedunculated polyps, are small flaps of extra skin. They’re harmless and typically cause no symptoms unless irritated by rubbing.
If skin tags become bothersome, a clinician can remove them surgically or with laser therapy.
Lichen sclerosus
Lichen sclerosus is an uncommon skin disorder that most often appears after menopause.
It primarily affects the vulva and the area around the anus. Possible symptoms include:
- intense itching
- white or pale discolored patches
- skin that tears easily
- bleeding or bruising
- pain with urination or intercourse
Topical corticosteroid creams or ointments are the usual treatments, but the condition can recur after therapy. People with lichen sclerosus have an increased risk of vulvar cancer.
Genital herpes
Genital herpes is caused by the herpes simplex virus (HSV) and spreads through close skin-to-skin contact.
Symptoms are often mild, and many infected individuals do not realize they have herpes.
When outbreaks occur, they may include:
- blistering sores or ulcers that may ooze or bleed
- pain, itching, or a tingling sensation
- fever
- swollen lymph nodes
Herpes symptoms typically resolve and then can recur. Over time, outbreaks usually become less frequent and less severe.
There is no cure for genital herpes, but antiviral medications can reduce the severity and duration of episodes.
Genital warts
Genital warts result from human papillomavirus (HPV) infection and spread via intimate skin-to-skin contact.
Many people with HPV-related warts are unaware of them. When symptoms appear, they may include:
- clusters of small, skin-colored bumps
- rough areas of closely packed warts, sometimes compared to a cauliflower
- itching or burning
There’s no definitive cure for genital warts, but treatments — including prescription creams, laser therapy, or surgical removal — can eliminate visible warts.
Certain HPV strains raise the risk of cervical cancer. If you have genital warts, see a clinician for a Pap test to determine the HPV type involved.
Cancer
Cancers of the vulva or vagina are uncommon. Signs of precancerous or cancerous lesions in these areas may include:
- abnormal bleeding
- unusual vaginal discharge
- noticeable lumps in the skin
- pain during intercourse
To confirm vulvar or vaginal cancer, a doctor will take a tissue biopsy from suspicious lesions for microscopic examination.
When to contact a healthcare professional
It’s wise to see a healthcare provider if you notice any new or persistent change to your body, including a lump that lasts for several weeks.
Various clinicians can evaluate and manage conditions of the vulva and vagina, such as your primary care physician or an obstetrician-gynecologist (OB-GYN).
Seek medical attention if you experience pain or signs of infection, for example:
- discharge from the lump that contains pus or blood
- symptoms suggestive of a sexually transmitted infection (STI), like itching, painful urination, or a rash
Quick home remedies to try
Most vaginal bumps and lumps can be managed at home. The following measures may ease symptoms:
- For cysts, take warm baths several times daily for a few days—warm water can encourage drainage.
- Use a sitz bath in the tub or on the toilet seat. If frequent full baths aren’t possible, a sitz bath can help soften cysts. Over-the-counter sitz bath kits are available at many pharmacies.
- Avoid clothing that rubs or chafes the vulva.
- Choose underwear made from natural fibers, like cotton, which are breathable and help keep the genital area cool and dry.
Bottom line
Lumps on or near the vagina are unlikely to be serious in most cases. Many resolve on their own or can be treated at home.
If you suspect an STI or have symptoms consistent with one, contact a healthcare professional for testing. Early treatment can reduce the chance of complications.
























Leave a Reply
You must be logged in to post a comment.