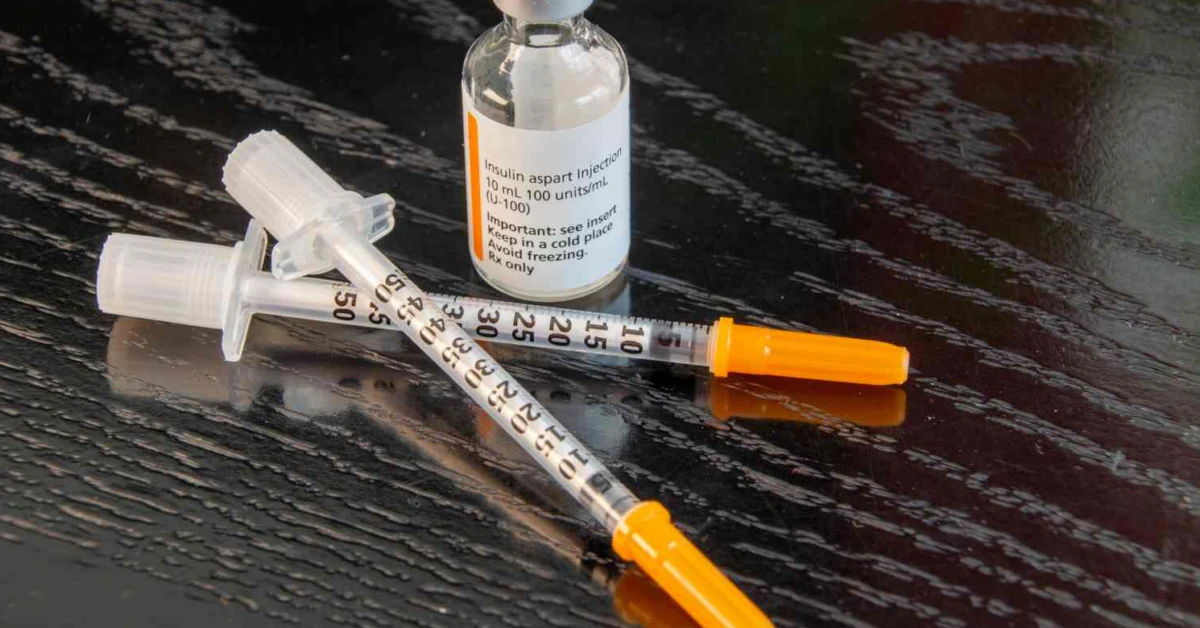
You’ve probably heard whispers about this new once-weekly insulin—and yeah, it’s legit. Let me break it down like we’re chatting over coffee:
Insulin efsitora (say it slow: eff-SEE-tora) is shaking things up for adults with type 2 diabetes. Recent research from the American Diabetes Association meeting shows it’s just as good at lowering HbA1c as insulin glargine, the once-daily standard. But here’s the kicker: You only inject it once a week. Imagine trading seven daily diabetic routine jabs for one weekly reminder. Sounds like a win, right?
Let me drop this: After 52 weeks (that’s a full year), A1C levels fell from 8.20% to 7.05% for efsitora users, while glargine shifted from 8.28% to 7.08%. Not a huge gap. In fact, the estimated treatment difference was –0.03 percentage points—which means they’re basically twins. Noninferiority? Check.
And get this: More people on efsitora hit that elusive <7% A1C goal (57% vs. 52%). So yeah, maybe this weekly insulin isn’t just easier—it pushes harder for better outcomes. Plus, the low blood sugar drama? Way less for efsitora people. Level 2/3 hypoglycemia dropped by 43% compared to daily insulin users. That’s a lighter load on the nerves, if you ask me.
Why You Should Care
You’re thinking, “But what does this mean for someone who doesn’t live and breathe diabetes stats all day?” Let me tell you a story to explain.
A Different Kind of Diabetes “Routine”
I know this woman named Karen. She’s a nurse. She’s got type 2 diabetes. She saw patients for 12 hours straight and then forgot her nightly insulin jab more times than she wants to admit. Repeating her dose made her anxious—she knew what low blood sugar could feel like: shaky, sweaty, and gut-wrenching. Exhilarating, not. But she needed that glargine to keep her A1C from spiraling.
When the QWINT trials dropped—trials testing this new once-weekly weekly insulin—Karen was all in.
“I didn’t want another routine to let me down,” she says. “This felt like reclaiming part of my life.”
So yeah, simplifying insulin treatment is more than a number on the screen. It’s real life, easier to manage. Basic yet life-changing, like setting one alarm instead of seven.
What’s the Deal with Insulin Efsitora Alfa?
Let me pop on my researcher hat for a sec, then I’ll shake it off and we’ll keep it real.
Efsitora (or insulin efsitora alfa) works like glargine. It’s a basal insulin, which is diabetes jargon for “background sugar control.” Type 2 diabetics often need it when their A1C is stubborn—think numbers above 7% after months of trying everything else.
In most cases, providers recommend starting daily basal shots (including glargine) to smooth out glucose peaks and dips. But let’s be real—getting that daily shot doesn’t exactly scream “convenient.” It’s easy to skip when life gets messy, work runs late, or you’re mentally maxed out.
That’s where once-weekly efsitora swoops in. It softens that big sticking point. And no, it’s not some dodgy game of shortcuts—they’ve actually tested it in humans (not just mice in labs).
The big study? It tracked over 1,800 adults for a year. Glargine vs. efsitora. Outcome? The weekly was just as effective and safer in the long run. Kudos to the New England Journal of Medicine, who published it back-to-back with ADA’s summit in June 2025.
| Category | Insulin Efsitora | Insulin Glargine |
| Injection Frequency | Once per week | Once per day |
| End A1C Level | From 8.20% to 7.05% | From 8.28% to 7.08% |
| Rate of Hypoglycemia | Lower by 43% | Higher (considering level 2/3 episodes) |
| Weekly Dosing Amount | Average 289.1 U/week | Average 332.8 U/week |
Source: data from the QWINT trials, as published in scientific circles: NEJM breakdown and PubMed’s review of efficacy.
And it’s fair to ask: Why wasn’t this developed sooner? Truth is, long-acting insulin took years to play with pharmacokinetics—the way the drug moves and works in your body. Efsitora? It builds on a smart delivery mechanism: fixed but flexible. Not too rigid, not too chaotic.
What’s a fixed regimen? Think of it as a deposit—same insulin amount each week. Think 100 Units. But—in trials, there was room to adjust up or down by 20%. So it’s not one-size-fits-all; you and your healthcare provider can tweak it over time.
Let’s Talk Numbers—Why HbA1c Matters
A1C levels tell us how a person’s blood sugar behaved over the last 2–3 months, like a report card for your glucose game. The ADA recommends getting it below 7% optimum for most people with type 2 diabetes. Efsitora made that happen for 57%, glargine for 52%. Not a huge gap, but movement in the right direction for folks who’ve struggled to hit the target before.
This is a win for quality of life, not just points on a graph. Low blood sugars (those scary <54 mg/dL moments) were slashed across the board when comparing weekly insulin to daily insulin glargine. Less pricks, fewer glucose crashes. Medical people refer to this as improved glucose control without the chaos.
Here’s the Puzzle: Why Is Weekly Insulin Targeting Lower Blood Sugar So Smart?
Quick refresher (without the textbook talk): When we run into low blood sugar drops, our brain reacts like, “Uhhh panic!” That means adrenaline spikes, heart races—it feels real bad. Worse? Some people stop using insulin because they’re scared of going too low—known as hypoglycemia avoidance.
But maybe efsitora changes that. With lower low blood sugar risk, it might keep you safer while keeping your sugar from going rogue. Many trials even suggest the A1c reduction was more consistent for people who didn’t want to inject daily (or couldn’t).
The Flipside: Is Once-Weekly Right for Everyone?
Okay, hold on. This isn’t a shortcut—it’s a smart strategy. Think of a carpenter swapping a hammer for a wrench. Both work, but one might do less damage to your thumb. Same way, efsitora’s clever weekly tool doesn’t guarantee wake-up calls for insulin newbies. Responsible talk with an experienced healthcare provider will unlock the potential.
Let’s talk safety. Adverse events were roughly equal in efsitora and glargine users—good news. But like any medication, if you’re not a textbook poster patient, keep in mind trials excluded things. For example, people with severe kidney disease or pregnant runners? Not in the studies. Keep that conversation open.
What About Side Effects and Cost?
No drug comes completely clean. But in these studies, both insulins landed neck-in-neck on safety. No scary side effects emerging among efsitora users. Not a red flag in sight—just solid data. Kinda rare for early trials.
Cost, though? That’s where the “real-messy-in-the-meds-world” mess comes in. Some type 2 diabetics I know walked away from it when dosing started because insurance didn’t roll with the punches. So yeah, while the potential is chill-free, money talks too.
Moving Beyond the “Daily Grind”
Now let’s talk lifestyle. Karen didn’t just switch insulin dosing; she backtracked from that weird mental cycle of daily injections = daily stress. Let’s put it this way: Imagine you had full access to a cake buffet every day, but you only wanted to eat cake once a week. For type 2 diabetics, taking shots daily feels like that forced plan.
But with efsitora? You get that once-a-week rhythm. Karen started counting her injections as a milestone, not a chore. She also got to around the overseas travel that made jabbing a surreal challenge. No refrigerator stabs. No pierce-and-pray when her med bag got packed last minute.
So yeah, this is more than efficiency—it’s about fitting into your own life without fireworks.
What’s It Like Switching from Glargine to Efsitora?
“Honestly? A relief,” Karen said. “I don’t have to track highs and lows as much anymore. It’s like my insulin finally gets me.”
Other folks I spoke to (and one massive study) confirm the same vibe: People report fewer surprises in their sugars. Oh yeah, and nearly 85% said they stuck to the plan easier. Low-literacy and younger crowds tend to find fixed-dose reliabilty easier, too. Some metforms tried once, twice. Still a tough habit to build—the end result matters more than the path.
This feels like shaping insulin therapy around you instead of you revamping your life for drugs. Good and smooth. I’ll take that combo all day long.
Should You Ask Your Provider About Efsitora?
Why not? If you’ve found yourself wrestling with daily insulin doses, or if your A1C’s been stubborn, efsitora might be the right help. But—and this is a but—it’s not miracle insulin. You’ve gotta start on the same track. Doctors still have to watch your needs closely.
What to Bring Up at the Doctor’s Office
- “Hey Doc, have you heard about this once-weekly option?”
- “I’ve missed doses before. Would a weekly treatment help?”
- nervous laugh “Can we test how this new insulin plays with my coffee habit?”
Jokes aside, real talk with your provider is key. It’s not a random swap—it’s part of a strategic set. Does your glucose fluctuate much during the week? Do you worry about nightly versus weekend habits? Does your body already scream to be left alone after daily shots? Bring it all up.
Remember: You can’t replug it in right away. Some folks need daily fine-tuning. But the QWINT trials? They suggest strong answers for most.
What’s Next? Is Weekly Insulin the New Normal?
Here’s the spoiler you didn’t know you needed: Experts think so. If you’ve seen these studies already—especially the New England Journal of Medicine report—you know this is a piece of a broader shift in type 2 diabetes care. The phrase “fixed-dose past daily insulin” is more than a headline. It’s slowly redefining standards, making life easier for over 37 million U.S. adults with type 2 diabetes.
Not quick to judge—but this is where you get to push up your sleeves and ask “What’s next?”. Because being dialed into your care matters. Being stable? No less. But turning months of prick-and-pray into one weekly plan? We all want to do better with less — especially on our $200-a-month med rollercoaster.
I rounded up real docs from this ADA news story. They’re leaning into weekly insulin as a potential gold standard soon—especially for patients who’ve been boxed in by daily jabs and shaky routines. Some think your insulin should make life convenient, not give you a side-eye when you try.
Why Should I Care How Diabetic Treatments Evolve?”
Because your care deserves flexibility. New research means you get more tools, more choices, and more options to live life like you want. If you’ve gotten down to 8% on metformin and glargine doesn’t make your numbers drop without a fight—maybe this once-weekly option sways the game?
The Takeaway
Insulin efsitora is giving type 2 diabetes survivors a clean, gentler shot at slower yet steadier A1C control. It lowers hypoglycemia drama. It gives hope to those stressed as hell over seven jab rounds. It doesn’t promise zero complications, but it yanks diabetes management down from the clouds, so you can grab it and run.
Efsitora isn’t cheating the system—it’s using science to meet you where you are.
So go ahead and bring this to your provider. No harm in asking. And if you’re curious about new diabetes marches? Drop some dollars into American Diabetes Association resources. Into sharing stories? Swing by Patient Diabetic Registries and connect with those who’ve taken their own shape through weekly insulin transitions. We need every ally and every tool along this path.






















Leave a Reply
You must be logged in to post a comment.