Here’s the big news: A clinical trial in 2025 showed that 10 out of 12 people with severe diabetes no longer needed insulin injections after just one year of stem cell therapy. Like, imagine – no more needles, no more endless monitoring. But let’s keep it real: Trials are small, costs are sky-high, and there’s still a ton we don’t know. We’ll unpack it all, easy peasy.
You’re probably asking, “Is this even real? How does stem cell therapy work for diabetes?” Great questions. Let me tell you what scientists are seeing, what patients are experiencing, and yes – even the risks no one’s shouting about yet.
The Trial That Left Experts Blown Away
A few months ago, I scrolled past a headline that made me pause: “10 out of 12 With Type 1 Diabetes Cured Through Stem Cells.” Cured? In 2025? It felt like science fiction. But here’s what went down: Researchers took donor stem cells, turned them into insulin-producing islet cells, and injected them into the liver. Most patients… stopped needing insulin. For a year. Even better, their blood sugar stayed stable over 98% of the time.
One guy, 59, with type 2 diabetes? He also ditched insulin. The study was tiny – only 12 patients – but this isn’t random luck. The team behind it included heavyweights like Dr. David Thompson (who’s been poking at this problem for 15 years) and researchers from Harvard and the Stem Cell Network.
Sounds too good to be true? Keep reading. We’ll break down the risks below, but first – let me explain how this actually works.
OK, So How’s This Stem Cell Jazz Even Work?
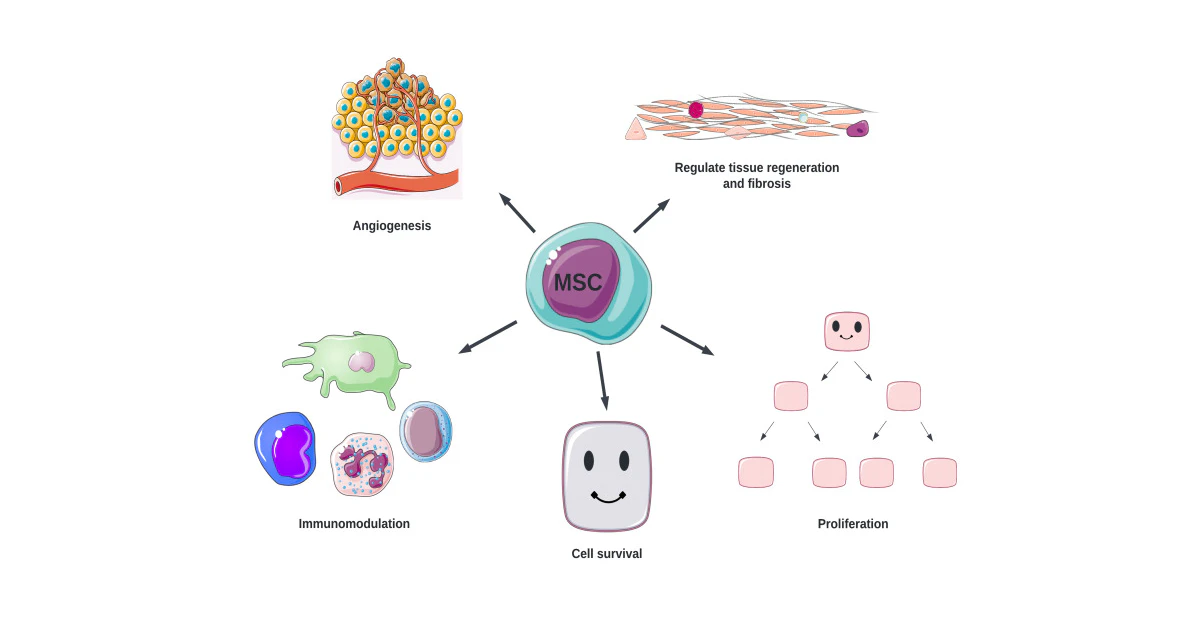
Let’s get geeky for a sec. The word “stem cell therapy diabetes” might sound like medical witchcraft, but the idea’s simple. Scientists either:
- Take a patient’s cells, reprogram them, and grow functional islet cells in a lab
- Use donor stem cells (often from pigs, yep) and tweak their genes to play nice with the human body
These cells get injected into your liver – where they start pumping out insulin like your pancreas forgot how to. But here’s the messy part: Your immune system might flip its lid, mistaking the new cells as attackers. That’s why some trials use genetically modified pig cells (per research from PMC), while others bank on “universal donor” cells that won’t set off alarm bells.
Animal Cells? Really?
“Wait, animal cells?” I hear you gasping. Yeah, pig islets are like the unsung heroes here. But not just any pigs – genetically-edited pigs.
You know how superheroes wear masks? Scientists gave pig islet cells a vague cosplay makeover using CRISPR edits. They knock out xenoantigens (which tell your body “I’M A STRANGER!”) and add human proteins like CD46 to help them blend in. It’s like teaching a pig cell to speak fluent “human immune system.”
Why pigs? Turns out, their insulin works eerily like ours. Science confirmed this after they tried everything from fish proteins to… well, let’s not talk about that. Point is: adult pigs give good islet yield. Neonatal pigs? Cheaper but less predictable. Fetal pigs? Basically ghosted the process for now.
Meet The Brains Behind This Madness
This isn’t just a random experiment done in a garage. We’re talking about some Gedanken (German for “brilliant thinking,” because why not throw in fancy words?) from the top diabetes nerds:
- Dr. David Thompson – The guy who led the Vancouver trial, making headlines with that 83% insulin-free number.
- Dr. Tim Kieffer – Known for shouting, “Beta cells shouldn’t quit on us!” He’s been engineering stem cells that act exactly like real ones for over a decade.
- Dr. Hannah Pizzato – Trying to figure out how to teach stem cells the art of vanishing from your immune system. University of Arizona badge of honor.
These folks aren’t chasing clickbait – they’re the brains running multi-million-dollar experiments. Their latest clinical breakthroughs have journals and hospital corridors buzzing like a coffee-addicted octogenarian.
Real People. Real Changes.
Let’s talk heart-thumping reality. A 25-year-old woman had enough of insulin armies chasing her blood sugar. She got islet cells from her own stem cells (personalized VIP treatment, basically). Within three months… she was making her own insulin. One year later? Still insulin-free. Total turnaround, straight outta beta cell boot camp.
The trial from PubMed’s got another epic story: 21 adults with type 1 diabetes in Brazil. Most were insulin-free for 3.5 years. One guy licked diabetes after eight years, which feels more like making peace with an old boss.
Who’s Eligible for These Trials?
If you’re geeking out and thinking, “Sign me up!”, let me slow you down with the hard truths:
- Most trials accept adults aged 20–50 first
- Only candidates with major insulin failures or hypoglycemic unawareness (like, your body stops screaming about sugar crashes – dangerous stuff)
- Insurance? Legal coverage? Not happening yet. These aren’t corner-store drugs.
If you’ve had diabetes diagnoses for more than 5 years with daily insulin chaos, maybe you’ll qualify. For now, these treatments are like golden tickets to Willy Wonka’s chocolate factory – rare, selective, and experimental. Artificial pancreases still feel more like a backup plan.
Pros and Cons – Let’s Tell You the Truth
| Stem Cell Sweat Equity | Daily Insulin World |
|---|---|
| Potentially one-time intervention | Daily injections forever |
| Pooling reports of “feeling normal again” | Forever dancing with highs/lows of blood sugar |
| Upfront costs weigh heavy: tens of thousands + experimental fees | Monthly meds, but cheaper than trial roulette |
| Real risks: infection/Acid-wash-treated blood counts (yes, that term comes from Canadian Cancer Society) | Risks: Injection-site drama, sugar swings |
Now, one year of insulin-free life? Golden goal. But let’s talk about whether your wallet and body can take the pressure. Trials keep showing promising stuff – but you might end up with side effects like low counts or infections if things go sideways. One patient at NYT actually said, “Side effects scared me at first, but going isolet-free made that fear shrink.”
So… Is This For Me?
If your diabetes feels like riding a greased rollercoaster without seat belts, stem cell therapy could maybe help. But let’s be frank: This isn’t off-the-shelf ‘magic bullet.’ Trials usually target patients with:
- Severe hyperglycemic or hypoglycemic events
- Pancreas that gave up the ghost
- Tried insulin pumps, ketones zones, fancy monitors – nothing plays nice
No shortcuts. You’ll need at least two dozen screenings (goodbye nap time), immune-suppressing drugs (your dashboard from this news source says), and buckets of patience. Early data showing hypoglycemic unawareness chance comeback within ~3 months. But not every story ends like TikTok viral memes. Some patients still poked themselves after 6 months
Forks in the Road Ahead
Okay, so if this treatment isn’t ready for mass dance floor yet – then what’s the hold-up? Good questions, keep waiting. Let’s zone in:
- Engineering drama: Making pig islet changes smooth enough that rejection nightmares don’t wake people up
- FDA timelines: Most trials still hush-hush – with close-to-2026 when big VX-880 results drop
- Location magic: Trials concentrated in places like Vancouver, Boston, and Sweden. No suburban pop-up clinics happening just yet
Though check this Nature study snippet: The phrase “2–3-fold higher cell doses” dropped, suggesting tweaks ahead. Suppose scientists aren’t perfecting forever – but they’re diving deep into sugar-starving cell territories.
Where’s This Going in 2025 and Beyond?
Speculative + What’s cooking in labs and boardrooms:
The “Off-the-Shelf” Stem Cell Wave
The holy grail? Universal donor cells working for anyone. Not need someone else’s pig insulin, not tailored VIP cells – just methods everyone can access. The Brown Lab up in Wisconsin might be onto this, as per this 2025 Press Release.
Rejection-Free Islets
no immunosuppressants (per this Swedish data) means you won’t have to swap one health maze for another. Like… being free from diabetes and side-effect pharmaceutical chuckle.
Sugar-Whispering Cells
We’re heading into gene-edited utopia where transplanted cells not just survive but refine their insulin responses. The future feels… different. Maybe we’ll whisper thanks to once-“destiny-predicted diabetic life” doctors, who stories started caving in early 2025.
Wait – Should I Be Freaking Out Over This?
Two Extremely Important Ps:
- This “diabetes cure” is still called experimental for solid reasons. Trials have seen insulin independence gains, but we can’t throw “safe”, friendly raises. Until long-term data drops, donors might vanish due to rejection. Or autoimmune reactions. Or side effects we haven’t titled yet.
- Treatment universe isn’t only for Type 1. Researchers rag about T2 risks differently – best results so far limited to severe insulin-dependent cases mostly seen in mixed T2 scenarios. Patients who nutrition and exercise can reverse… should hold off.
Final Words
In case you’re feeling sandwiched between hope and hot air – right. Effectiveness studies are promising but growing science cabbage from a headstart. If your “Omg more patients need to cover” crib notes – they’re right, and curative estimates still resemble batch bread dough, not boxed perfection yet.
If you’re walking down severe diabetes street, have a chinwag with your doctor about available clinical trial registries. These therapies aren’t “revolutionary” light switches but evolving. Volunteering could mean anonymously steering the wheel toward universal options – for everyone.
Got questions? Scaredly curious? Drop your and angst in the comments. We’re all straddling science and stories together.





















Leave a Reply
You must be logged in to post a comment.