Short answer: tingling isn’t one of the classic hallmarks of ALS, but in a surprising minority of patients it can show up, usually because something else is happening alongside the disease. If you’ve ever felt that “pins‑and‑needles” buzz in your fingers and wondered whether it could be ALS, you’re not alone – the question comes up more often than you might think.
Let’s dive into what the science really says, why doctors ask you about tingling, and what steps you can take right now. I’ll keep it friendly, straightforward, and sprinkle in a few real‑world stories so you don’t feel like you’re reading a textbook.
Typical ALS Signs
First, it helps to know what ALS usually looks like. ALS (amyotrophic lateral sclerosis) is a progressive motor‑neuron disease. The nerve cells that tell your muscles to move slowly die off, so the most common symptoms are purely motor:
- Muscle weakness, often starting in a hand, foot, or voice box.
- Fasciculations – those tiny, involuntary muscle twitches you sometimes see under the skin.
- Muscle cramps and stiffness (spasticity).
- Difficulty speaking, chewing, or swallowing as the disease spreads.
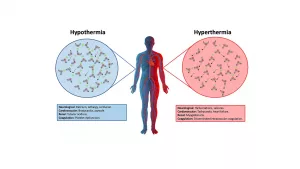
Because the disease attacks the motor system, the classic definition of ALS does not include sensory loss – you shouldn’t expect numbness or tingling as a primary sign. That’s why neurologists often ask “Do you have any numbness or tingling?” as a way to rule out other conditions.
Tingling in ALS
So why do some patients report a tingling feeling? It turns out the picture is a little messier than the textbook description.
In a 1996 Korean Neurological Association study of 77 ALS patients, about 32.5 % said they experienced paresthesia – that’s the fancy medical term for tingling, pins‑and‑needles, or a “buzzing” sensation. Only five of those patients had an obvious second diagnosis such as cervical radiculopathy or peripheral neuropathy, suggesting that a small subset of ALS patients truly feel a tingling symptom without another clear cause. according to a 1996 Korean Neurological Association study, sensory changes can arise from subtle degeneration in central sensory pathways.
More recently, the ALS United guide on early symptoms mentions that while tingling is not typical, “early sensory complaints have been reported in up to one‑third of patients, often alongside other motor signs.” The same guide stresses that early detection of any new sensation should prompt a thorough neurologic work‑up because early intervention can improve quality of life, even if the tingling itself isn’t treatable directly. the ALS United guide also notes that many patients describe the sensation as an “electric” or “hum” feeling—something you’ll see echoed in personal stories on ALS forums.
Here’s a quick snapshot from a forum thread where a member described an “electric feeling in nerves” that lingered for months before a formal diagnosis. The community response was a mix of reassurance (“it’s not typical, but it can happen”) and practical advice (check for cervical spine issues first). Seeing real voices helps remind us that data points are lived experiences.
Case‑Study Snapshots
| Patient (pseudonym) | Age | Primary ALS sign | Tingling description | Additional finding |
|---|---|---|---|---|
| DaveJ | 58 | Hand weakness, fasciculations | Buzzing sensation in the forearm, “like a phone on vibrate” | EMG confirmed ALS; MRI normal |
| Farfalla | 67 | Progressive muscle weakness in fingers | Intermittent “pins and needles” in index and little fingers | Cervical radiculopathy discovered on imaging |
Other Causes of Tingling
If you’re feeling that uncomfortable buzz, it could be anything from a harmless posture glitch to a chronic medical condition. Below are the most common culprits that often get confused with ALS:
- Diabetic peripheral neuropathy: High blood sugar can damage the tiny nerves in your feet and hands, leading to persistent tingling.
- Cervical radiculopathy: A slipped disc or bone spur in the neck can pinch nerve roots, creating a “electric” feeling that radiates down the arm.
- Peripheral neuropathy from vitamin deficiencies: Low B12, vitamin D, or folate can produce similar symptoms.
- Lyme disease: The bacterium that causes Lyme can mimic many neurological issues, including tingling, especially early on.
- Medication side effects: Certain chemo agents, antiretrovirals, or even some blood pressure meds can tingle your nerves.
Red‑flag patterns that usually point away from ALS include symmetrical tingling in both hands or feet, loss of temperature sensation, and a gradual progression over months rather than a sudden onset with motor weakness.
Comparison Chart
| Feature | ALS‑Related Tingling | Diabetic Neuropathy | Cervical Radiculopathy |
|---|---|---|---|
| Typical onset | Often accompanies motor weakness | Gradual, feet first | After neck injury or posture strain |
| Distribution | Focal, often unilateral | Bilateral, stocking‑glove pattern | Unilateral, follows nerve root |
| Associated motor signs | Fasciculations, weakness | Usually absent early | May have muscle atrophy of the arm |
| Diagnostic clue | EMG shows motor‑neuron loss, no sensory nerve‑conduction delay | Reduced nerve‑conduction velocity | MRI shows disc herniation |
Doctor’s Evaluation
When you bring tingling to a neurologist, expect a systematic approach. The exam often starts with a few key questions:
- When did the tingling start, and how has it changed?
- Is it associated with any weakness or muscle cramps?
- Do you have diabetes, recent injuries, or a history of Lyme disease?
After the interview, the doctor will run a series of tests:
- Electromyography (EMG) and Nerve Conduction Studies (NCS): EMG reveals motor‑neuron loss typical of ALS; NCS can detect peripheral nerve damage that would explain tingling.
- MRI of the brain and cervical spine: Helps rule out structural problems like radiculopathy or tumors.
- Blood work: Looks for diabetes, vitamin deficiencies, inflammatory markers, and infections such as Lyme.
According to ALS United, early diagnostic evaluation is crucial because it opens the door to multidisciplinary care and potentially clinical trial enrollment. the ALS United guide emphasizes that a thorough work‑up can separate ALS from treatable mimics, saving patients from unnecessary anxiety.
Decision Flow
Think of the evaluation as a simple flowchart: tingling present → detailed history → EMG/NCS → if motor‑neuron loss without sensory deficit → ALS diagnosis; otherwise → investigate other causes.
Managing Tingling (Even If It’s Not ALS)
Whether the tingling is part of ALS or an unrelated issue, there are practical steps you can take right now to feel better.
Lifestyle Tweaks
- Posture check: Spend a few minutes each hour standing up, stretching your neck, and adjusting your workstation. Small changes can relieve pressure on cervical nerves.
- Blood‑sugar control: If you have diabetes, keep your glucose numbers stable; tight control slows nerve damage.
- Hydration and nutrition: Proper electrolytes support nerve function, and a balanced diet provides the vitamins your nerves love.
Therapy & Rehab
Physical and occupational therapists can teach you gentle exercises that improve circulation and reduce the “electric” feeling in your limbs. Many ALS clinics also offer massage or neuro‑feedback techniques that many patients find soothing.
Medication Options
If the tingling is truly neuropathic, doctors sometimes prescribe gabapentin or pregabalin. These aren’t cures, but they can dull the sensation enough to let you focus on daily life. Always discuss the risks and benefits with your neurologist.
Key Takeaways
To wrap it all up, here’s what you should remember:
- Tingling is not a hallmark ALS symptom, but it can appear in a minority of patients, especially when another nerve issue co‑exists.
- Common alternative explanations include diabetes, cervical radiculopathy, vitamin deficiencies, and infections like Lyme disease.
- A thorough neurologic evaluation—EMG, MRI, blood work—will help pinpoint the cause and guide treatment.
- Even if the tingling isn’t ALS, lifestyle adjustments, therapy, and possibly medication can bring relief.
Remember, knowledge is power. If you notice persistent tingling, especially alongside any muscle weakness or twitching, schedule an appointment with a neurologist sooner rather than later. Early evaluation not only clarifies the cause but also connects you with the right specialists and support resources.
We’ve covered a lot, and I hope you feel a little more confident navigating this confusing symptom. Have you or someone you know experienced tingling and wondered about ALS? Share your story in the comments—your experience might just help the next person who’s scrolling through the same question.























Leave a Reply
You must be logged in to post a comment.