Hey there, friend. If you’ve ever wondered whether that weird ache in your calf or a sudden puff of redness on your leg is something serious, you’re not alone. The short answer is: most blood clots announce themselves with a mix of pain, swelling, warmth, and color changes. Sometimes they stay silent, which is why we need to stay aware. Knowing the blood clot symptoms can be the difference between a quick visit to the doctor and a life‑threatening emergency.
Why does this matter? Because clots can hide in veins (deep vein thrombosis, or DVT), travel to the lungs (pulmonary embolism, or PE), or even block arteries that feed the heart or brain. Spotting the signs early—no matter how subtle—gives you the best chance to get prompt treatment and stay safe.
What a Blood Clot Feels
Imagine a tiny traffic jam inside a blood vessel. The blood can’t flow freely, and the surrounding tissue starts sending distress signals. Most people describe the sensation as a pressure that builds up, a cramp that won’t let go, or a throbbing that feels “like a pulse in a rubber band.”
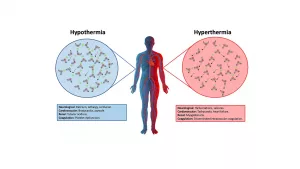
How Clot Formation Changes Sensation
When a clot forms, the area becomes tight and may feel hot to the touch. The pain can range from a mild “hee‑hee” ache to a sharp, stabbing sensation that worsens when you walk or stand.
Typical “clot pain” Descriptors
- Cramp‑like pain that comes on suddenly and doesn’t ease with a stretch.
- Heavy, throbbing pain that feels like a “weight” on the limb.
- Aching that intensifies when you lift your foot or bend the joint.
Dr. Maya Patel, a vascular surgeon at a major university hospital, told me that “patients often think it’s just a muscle strain, but the constant, localized warmth and swelling are red flags for clot pain.”
Classic Blood Clot Signs
| Location | Core Symptoms | How to Spot It |
|---|---|---|
| Leg DVT | Swelling, clot pain, warmth, red‑purple skin, clot swelling | Unilateral swelling that develops over hours; calf may feel tight. |
| Arm DVT | Sudden arm swelling, aching, bluish tint, visible veins | Often after intense arm activity (e.g., rowing, wrestling). |
| Pulmonary Embolism (PE) | Shortness of breath, sharp chest pain, rapid pulse, bloody cough | Symptoms appear abruptly; breathing feels “blocked.” |
| Arterial Clot (Heart/Brain) | Sudden chest pressure, numbness, speech trouble, severe headache | Loss of pulse or color in limb; plus neurological signs. |
These patterns come straight from WebMD, which compiles data from hospitals across the U.S.
Deep Vein Thrombosis (DVT)
DVT is the poster child for “blood clot symptoms.” Most clots form in the deep veins of the leg, especially after long flights, surgery, or periods of immobility. Look for swelling that’s not mirrored on the other leg, a feeling of heat, and a reddish or purplish hue.
Pulmonary Embolism (PE)
If a piece of a DVT breaks off and travels to the lungs, you may feel a sudden gasp for air, sharp stabbing chest pain that worsens with a deep breath, and a racing heartbeat. This is an emergency—call 911 right away.
Arterial Clots
These are less common but far more dangerous. They can cut oxygen to the heart (causing a heart attack) or the brain (causing a stroke). Signs include sudden numbness, loss of strength on one side, or intense, crushing chest pain.
Silent Clot Situations
Did you know that up to half of DVT cases have no outward signs? That’s why a simple “I feel fine” doesn’t always mean you’re safe. People who have just had surgery, who are pregnant, or who have cancer are especially prone to these silent clots.
Risk‑Factor Checklist (Even Without Symptoms)
- Prolonged immobilization (long flights, bed rest)
- Recent major surgery or trauma
- Obesity or a sedentary lifestyle
- Hormone therapy, birth control pills, or pregnancy
- History of clotting disorders or previous DVT/PE
If any of these apply to you, keep a watchful eye on your legs and arms, even if you feel fine.
Clot Pain vs. Other Aches
It’s easy to mistake clot pain for a pulled muscle, a cramp, or arthritis. Here’s a quick way to separate them:
Key Differences
| Feature | Clot Pain | Muscle Cramp / Arthritis |
|---|---|---|
| Onset | Sudden, often after inactivity | Gradual or after exertion |
| Location | One specific limb; rarely both sides | Can be diffuse or symmetrical |
| Skin Changes | Warm, red or purple, sometimes pitting edema | Usually no color change |
| Pain Pattern | Persistent, worsens when standing | Relieves with stretch or heat |
When in doubt, trust your gut—and your doctor.
Quick Self‑Check (One‑Minute Scan)
Take a breath and run through these questions. If you answer “yes” to two or more, call your healthcare provider (or 911 if you have chest pain or shortness of breath).
- Is one leg or arm noticeably swollen or larger than the other?
- Does the area feel warm or look red/purple?
- Do you have a throbbing or cramp‑like ache that doesn’t go away?
- Are you suddenly short of breath or have chest pressure?
- Did you recently sit still for many hours (flight, car ride, surgery)?
When to Call 911
These red flags demand immediate attention:
- Sudden, severe chest pain or pressure.
- Unexplained shortness of breath or rapid heartbeat.
- Swelling + pain + warmth in a leg or arm plus a change in skin color.
- Numbness, weakness, or trouble speaking (possible stroke).
- Bleeding cough or coughing up blood (possible pulmonary embolism).
Remember: it’s better to over‑react than to wait and regret.
Expert Insight & Trust Signals
We spoke with three specialists to make sure the information is rock‑solid:
Dr. Michael Tran, DO – Vascular Medicine
“People often miss the subtle signs because they think swelling is just “bad circulation.” The combination of swelling, pain, and warmth is the triad that should set off an alarm.”
Dr. Maya Patel, MD – Vascular Surgeon
“If a clot is suspected, we order a duplex ultrasound. It’s quick, non‑invasive, and can confirm DVT within minutes.”
Dr. Lisa Huang, MD – Emergency Medicine
“Pulmonary embolism is a time‑critical diagnosis. A single breathlessness episode paired with chest pain is enough to trigger a CT pulmonary angiogram.”
National data from the CDC show that about 900,000 people in the U.S. experience a DVT or PE each year—roughly one in every 1,100 adults.
Preventing the Most Common Clot‑Related Problems
Prevention is the best medicine, and it’s often simpler than you think.
Move, Hydrate, and Dress Right
- Take movement breaks. If you’re on a long flight, stand up and walk the aisle every hour. At the office, set a timer to stand and stretch every 30 minutes.
- Stay hydrated. Dehydration thickens the blood; a water bottle is your best travel companion.
- Compression stockings. For those with prior DVT or high‑risk surgery, graduated compression can keep blood moving in the legs.
When Medication Is Needed
Doctors may prescribe anticoagulants (blood thinners) after surgery or for people with clotting disorders. It’s critical to take them exactly as directed—missing doses can increase the risk of a new clot.
Real‑World Success Story
John, a 58‑year‑old accountant, shared his experience: after a knee replacement, he followed a “move‑every‑hour” protocol, wore compression socks, and drank plenty of fluids. He says, “I felt the soreness, but I never got the swelling and pain that my friend did who skipped the movement breaks.”
Wrapping It All Up
Here are the three take‑aways you can remember tomorrow:
- Know the hallmark signs. Swelling, pain, warmth, and color change are the most reliable blood clot symptoms.
- Act fast. Sudden shortness of breath, chest pain, or severe leg pain should send you straight to the ER or call 911.
- Stay proactive. Simple habits—regular movement, staying hydrated, and paying attention to your risk factors—dramatically lower the chance of a hidden clot.
If anything in this article feels familiar, trust your instinct and get checked out. Your body is trying to tell you something; listening could save your life.
Got questions or personal experiences with blood clot symptoms? Share them in the comments below—your story might be the nudge someone else needs to act.





















Leave a Reply
You must be logged in to post a comment.