If you’re 45 or older, a colon cancer screening test can catch precancerous polyps or early‑stage cancer before any symptoms show up. The good news? There are several safe options—colonoscopies, FIT kits, stool‑DNA tests, CT colonography, and more—so you can pick the one that fits your life.
Choosing the right test feels a bit like shopping for the perfect pair of shoes: you want comfort, reliability, and a style you’ll actually wear. Let’s walk through the choices together, talk about the pros and cons, and figure out which screening test will give you peace of mind.
Why Screening Matters
“Screening” simply means looking for disease in people who feel fine. For colorectal cancer, that early glance can shave years off a potential diagnosis. In 2024, roughly 152,810 Americans were expected to receive a colon cancer diagnosis, and almost 53,000 were projected to die from it — a stark reminder that early detection saves lives (according to the National Cancer Institute).
When polyps are removed during a screening, they never get the chance to turn malignant. Studies show that regular screening can cut colorectal‑cancer mortality by about 60 % — a number that feels reassuring, especially when you consider how many lives could be saved with a simple test.
Types of Screening Options
Below is a quick snapshot of the most common, FDA‑approved tests. We’ll dig deeper into each after the table, but this overview can help you spot the one that feels right.
| Test | How It Works | Frequency | Key Pros | Key Cons |
|---|---|---|---|---|
| Colonoscopy | Tube with camera examines entire colon | Every 10 years | Detects & removes polyps in one visit | Invasive, prep required, rare complications |
| FIT (Fecal Immunochemical Test) | Stool sample checks hidden blood | Yearly | At‑home, no diet restrictions | Less sensitive to small polyps, needs follow‑up colonoscopy if positive |
| Stool DNA Test (FIT‑DNA, e.g., Cologuard) | Detects blood + DNA changes in stool | Every 3 years | Higher sensitivity than FIT alone | More expensive, still requires colonoscopy if abnormal |
| CT Colonography (Virtual Colonoscopy) | Low‑dose CT creates 3‑D colon map | Every 5 years | No sedation, shorter procedure | Radiation exposure, still needs colonoscopy for any positive finding |
| Flexible Sigmoidoscopy | Shorter scope visualizes lower colon | Every 5 years (or 10 years + FIT) | Less prep, quicker than full colonoscopy | Only checks part of the colon, may miss upper lesions |
Choosing the Right Test
Think of this step like a mini‑quiz you ask yourself before a doctor’s appointment:
- How much prep are you comfortable with? Colonoscopies demand a thorough bowel cleanse; FIT or stool‑DNA kits just need a small sample.
- Do you prefer a one‑time thorough exam or repeated at‑home checks? A colonoscopy is a “set‑and‑forget” for a decade. FIT is yearly, which can feel less daunting for busy schedules.
- What does your insurance cover? Most plans cover colonoscopies, FIT, and stool‑DNA tests, but out‑of‑pocket costs vary. Check with your insurer early (a study by the CDC notes that coverage differences often drive patient choice).
- Any personal risk factors? Family history, inflammatory bowel disease, or genetic syndromes may tip the scale toward a colonoscopy or earlier start.
One friend of mine, “Jen,” turned 52, worked two jobs, and dreaded the idea of a full colonoscopy. She opted for an annual FIT kit, mailed it in from her office break room, and felt relieved that a simple stool sample could keep her on track. When her FIT came back positive, she seamlessly moved to a colonoscopy—nothing fell through the cracks.
Benefits vs. Risks
Every screening test carries both rewards and downsides. Understanding them helps you make a confident decision.
- Early detection – All tests aim to find cancer before symptoms appear, dramatically improving treatment success.
- Procedural risks – Colonoscopies have a <0.1 % chance of perforation and a small sedation risk; FIT and stool‑DNA have virtually no physical risk.
- False positives – Stool‑based tests can flag blood from non‑cancer sources, leading to an extra colonoscopy you might not have needed.
- False negatives – No test is perfect. FIT may miss small polyps; CT colonography can miss flat lesions.
Balancing these points is where the “trust” factor shines. The American Cancer Society emphasizes that the most important step is simply getting screened, no matter which test you choose (according to ACS).
What to Expect on Test Day
Bowel preparation is the most universally dreaded part. You’ll either drink a polyethylene glycol solution (the clear, salty sip that looks like “slime”) or follow a water‑only regimen. Pro tip: chill the solution, sip slowly, and keep a bucket of ice nearby. Many people report that the “slime” taste fades after the first few minutes, and the relief afterward feels like a mini‑victory.
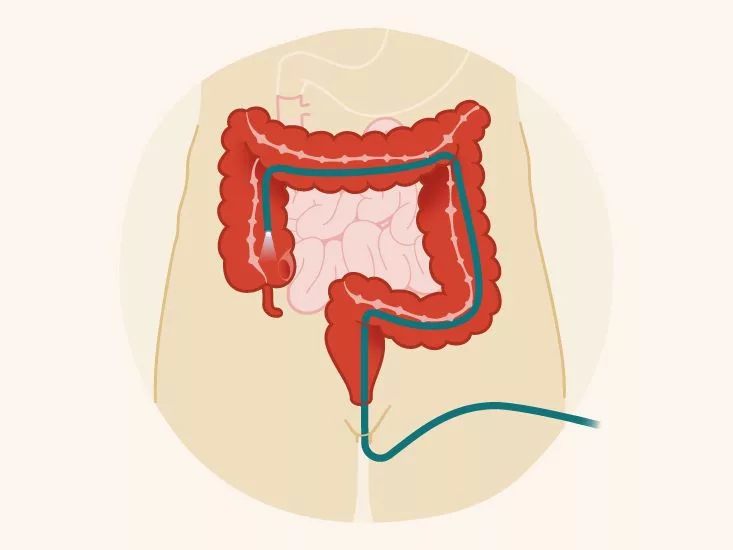
Colonoscopy experience usually goes like this: you arrive, change into a gown, get a mild sedative, and lie on your side while the doctor gently glides a lighted tube through your rectum. The whole exam lasts 30‑45 minutes, but you’ll spend another hour or two in recovery. Most patients describe the sensation as “numb and relaxed,” and you’ll be sent home with a simple set of post‑procedure instructions—no heavy lifting for 24 hours, and a soft‑food diet for a day.
For FIT and stool‑DNA kits, the steps are delightfully minimal: receive a kit, collect a small stool sample using a brush or spatula, seal it in the provided tube, and mail it back. No prep, no sedation, just a few minutes of effort. Scores of patients say the at‑home test lets them keep their privacy intact, which is a big comfort factor.
CT colonography feels like a quick CT scan at the radiology suite. You still need the bowel prep, but there’s no scope or sedation. The scanner whirs, creates a 3‑D image, and a radiologist reviews it within a day. If something looks odd, your doctor will schedule a follow‑up colonoscopy.
Who Should Get Screened & When to Start
The U.S. Preventive Services Task Force (USPSTF) recommends routine screening for average‑risk adults aged 45 to 75. If you’re over 75, the decision becomes personal—talk to your doctor about life expectancy and overall health.
Start earlier if any of these apply:
- First‑degree relative diagnosed before age 60.
- Two or more relatives with colorectal cancer or advanced polyps.
- Personal history of inflammatory bowel disease (Crohn’s or ulcerative colitis).
- Known genetic syndrome such as Lynch syndrome or familial adenomatous polyposis.
For high‑risk individuals, a colonoscopy often becomes the preferred choice, sometimes beginning at age 40 or even younger. The CDC’s screening guidelines reinforce that a personalized approach—guided by family history, lifestyle, and medical conditions—yields the best outcomes (according to CDC).
Bottom Line – Take Action Today
There’s no “one‑size‑fits‑all” answer when it comes to colon cancer screening tests. The most important thing is to pick a test you’ll actually complete. Whether you schedule a colonoscopy, order a yearly FIT kit, or try a stool‑DNA test every three years, the goal is the same: catch any trouble early, when it’s easiest to treat.
- Know your options. Review the table above, ask your doctor about pros and cons.
- Match the test to your lifestyle. Busy schedule? FIT might be your best friend.
- Talk to your healthcare provider. Bring up your family history, insurance coverage, and any worries you have.
Ready to take the first step? Call your primary‑care office this month and ask, “Which colon cancer screening test is best for me?” You’ll feel empowered, and you’ll be doing something truly loving for yourself and your loved ones.
Have you already tried one of these tests? What was the experience like? Share your thoughts in the comments below—your story could help someone else decide what’s right for them.






















Leave a Reply
You must be logged in to post a comment.