Short answer: once you’ve gone a full year without a period, you’re officially post‑menopausal, and a “regular” period will not return. If you notice any bleeding after that point, it’s a signal your body is trying to tell you something, and it’s worth getting checked out right away.
Why does this matter? Because post‑menopausal bleeding can be a harmless “false alarm” or a sign of something that needs attention, like an endometrial polyp or, in rarer cases, cancer. Knowing the difference saves you worry, unnecessary trips to the doctor, and—most importantly—keeps you in control of your health.
Quick Answer
Can you get a period again?
No, you can’t have a true menstrual cycle after menopause. The ovaries have stopped releasing eggs and the estrogen‑progesterone dance that fuels the uterine lining is over. Without that hormonal rhythm, there’s nothing left to shed each month.
What exactly is “postmenopausal bleeding”?
Any spotting, spotting, or heavier flow that happens after you’ve been 12 months without a period is called postmenopausal bleeding. It’s a broad term that covers everything from a tiny pinkish spot on a panty liner to a gush that would make you reach for a tampon.
The biology behind the final curtain
During the reproductive years, estrogen thickens the uterine lining (the endometrium) while progesterone steadies it. When you hit menopause, estrogen drops dramatically and progesterone disappears. The lining thins and eventually stays thin, so there’s nothing left to slough off. That’s why a “real” period simply can’t make a comeback. (Healthdirect explains the hormonal shift)
Why Bleeding Occurs
Common “menopause bleeding causes”
Bleeding after menopause isn’t normal, but it isn’t automatically scary either. Here are the most frequent culprits, listed from most benign to most urgent.
| Cause | What It Looks Like | Typical Work‑up |
|---|---|---|
| Endometrial atrophy or polyps | Light spotting, sometimes pinkish | Transvaginal ultrasound, possible hysteroscopy |
| Hormone‑therapy breakthrough bleeding | Irregular spotting while on HRT | Review dosage, consider switching formulation |
| Genitourinary Syndrome of Menopause (GSM) | Dryness, irritation, occasional spotting after intercourse | Clinical exam, vaginal estrogen therapy |
| Medication side‑effects (e.g., anticoagulants) | More prolonged bleeding, bruising elsewhere | Medication review, possible dosage adjustment |
| Uterine (endometrial) cancer | Heavy, persistent bleeding, sometimes with pain | Biopsy, referral to a gynecologic oncologist |
What about a “late menopause period”?
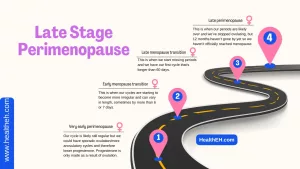
Sometimes women experience a very gradual transition where occasional spotting dribbles in during the final months before the official 12‑month mark. This is often just the tail‑end of the hormonal decline and isn’t a true period. However, once the 12‑month threshold is crossed, any new spotting moves into the postmenopausal bleeding category and deserves a look.
Genitourinary Syndrome of Menopause (GSM)
GSM affects up to 70 % of post‑menopausal women, causing vaginal dryness, itching, and even light bleeding after sex. It’s a chronic condition that worsens over time if left untreated. New Zealand’s Menopause Society highlights that early treatment with low‑dose vaginal estrogen can halt progression and improve comfort.
What To Do
When should you call the doctor?
Any bleeding after the 12‑month mark is a red flag. Even a single pink speck should prompt a call, especially if it’s accompanied by:
- Persistent spotting for more than a week
- Unusual odor or clotting
- Pain, especially pelvic or abdominal
- Recent changes in medication
Don’t wait for the “mountain” to become an “avalanche”—early evaluation is the safest route.
Typical diagnostic pathway
Doctors follow a step‑by‑step checklist to pinpoint the source:
- Pelvic examination – a hands‑on look at the uterus, cervix, and vagina. Healthdirect recommends this as the first line of assessment for any abnormal bleeding.
- Transvaginal ultrasound – a quick, non‑invasive scan that images the endometrium. Cleveland Clinic notes this is the go‑to imaging test for postmenopausal bleeding.
- Endometrial biopsy – a tiny tissue sample taken from the uterine lining, usually done if the lining looks thick (>5 mm) on ultrasound.
- Blood work – CBC to rule out anemia, thyroid panel, and sometimes hormone levels to see if any residual estrogen is causing a “breakthrough” bleed.
- Referral – if cancer is suspected, a gynecologic oncologist steps in for further staging.
Managing the cause
Once the underlying reason is identified, treatment varies:
- Polyps or fibroids – removed hysteroscopically, often in a single office visit.
- Hormone‑therapy breakthrough – adjusting the dose, switching from oral to patch, or adding a progestin can calm the lining.
- GSM – vaginal moisturizers, low‑dose estrogen creams, or non‑hormonal options like moisturising gels.
- Medication review – discussing blood‑thinners with your prescriber.
- Cancer – surgery, radiation, or hormone‑blocking drugs, depending on stage.
Staying Healthy
Long‑term health risks
Even though the period itself is gone, post‑menopause brings new health considerations that deserve attention in your menopause health guide. The biggest ones are:
- Cardiovascular disease – Estrogen protects artery walls; without it, the risk of heart attack and stroke rises. NHS Inform explains the importance of heart‑healthy habits after menopause.
- Osteoporosis – Bone density drops quickly in the first few years post‑menopause. Aim for 1,200 mg of calcium and 800–1,000 IU of vitamin D daily, plus weight‑bearing exercise.
- Urinary‑tract infections & incontinence – The drop in estrogen weakens pelvic floor muscles. Regular Kegel exercises and staying hydrated help.
Lifestyle and prevention
Think of your body as a garden. After the “season” of menstruation ends, you still need to water, prune, and protect it.
- Eat the rainbow – Plenty of leafy greens, berries, and fatty fish for antioxidants and omega‑3s.
- Move daily – Brisk walking, dancing, or yoga keeps the heart and bones strong.
- Screen regularly – Annual mammograms, a pelvic exam at least once a year, and a bone‑density test every 2–3 years after age 65 (or earlier if you have risk factors).
- Consider HRT wisely – Low‑dose estrogen can relieve GSM, protect bone, and improve quality of life, but it isn’t right for everyone. A board‑certified OB‑GYN can help weigh the pros and cons.
Quick checklist for your next doctor visit
- Note the date, amount, and color of any bleeding.
- List new or changed medications.
- Bring a brief timeline of menopause symptoms (hot flashes, sleep changes, etc.).
- Ask about the need for an ultrasound or biopsy based on your symptoms.
Real‑World Stories
Jane’s pink surprise
Jane, 58, thought a faint pink streak on a panty liner was just “old‑age spotting.” She booked a quick appointment, got a transvaginal ultrasound, and discovered a 1 cm endometrial polyp. The polyp was removed in‑office, and the bleeding stopped instantly. “I was terrified at first,” Jane says, “but the doctor’s calm explanation made everything feel manageable.”
Dr. Patel’s clinical tip
Dr. Maya Patel, an OB‑GYN with 15 years of experience, emphasizes that most postmenopausal bleeding cases are benign. “The key is not to dismiss the bleed, but also not to jump to the worst‑case scenario,” she notes. She recommends a single‑visit “bleed pathway” where the pelvic exam and ultrasound happen back‑to‑back, reducing anxiety and speeding up diagnosis.
Mike’s supportive partner
While the article focuses on women, Mike, a husband of a 62‑year‑old who experienced postmenopausal spotting, shares how he helped: “I reminded her to write down what she saw, drove her to the clinic, and stayed with her during the ultrasound. Knowing I was there made the whole process less scary for both of us.”
Wrapping It Up
In a nutshell, you won’t get a regular period again after menopause—that’s a biological fact. However, any bleeding after that point is your body’s way of waving a flag, and it’s worth listening. From harmless polyps to the less common but serious possibility of cancer, the spectrum is wide, but the first step is always a conversation with your doctor.
Take charge of your post‑menopausal health by staying active, eating well, keeping up with screenings, and knowing when to seek help. And remember—just like you’d call a friend when you notice something odd, you deserve a caring, knowledgeable professional on the other end of the line.
What’s your experience with postmenopausal bleeding? Have you found a tip that helped you stay on top of your health? Share your story in the comments, or reach out to a healthcare provider if you notice anything unexpected. You’re not alone, and together we can keep this journey as smooth as possible.






















Leave a Reply
You must be logged in to post a comment.