Quick answer: Seeing blood in your stool isn’t a classic sign of irritable‑bowel syndrome, but the way IBS twists your gut can set the stage for small injuries that bleed. If the blood is bright red, it’s usually a low‑down‑range issue like a hemorrhoid or a tiny tear. Dark or black stool signals a higher‑up bleed and deserves a prompt medical look‑over.
Bottom line: you don’t have to panic the moment you spot a speck of crimson, but you do need to know when a symptom is just a side‑effect of IBS and when it could be something more serious. Let’s break it down together, step by step.
Why Blood Isn’t a Direct IBS Symptom
What IBS Actually Does
IBS is a functional disorder – it messes with how your gut moves, but it doesn’t usually cause visible damage. The hallmark trio is:
- Abdominal cramping that eases after a bathroom trip
- Changes in stool consistency (diarrhea, constipation, or alternating between the two)
- Uncomfortable bloating or gas
These symptoms can be relentless, but the gut lining itself stays intact, which is why “blood in stool” isn’t listed as a core IBS symptom.
Medical Consensus – “Not a Direct Symptom”
According to Healthline (2025), blood in the stool is not a direct symptom of IBS. The article points out that while IBS can lead to conditions that cause bleeding, the syndrome itself doesn’t tear the intestine.
Key Study Insight
A 2023 systematic review discovered that 22 % of people with IBS‑C (constipation‑predominant) develop hemorrhoids because chronic straining irritates the anal veins. That’s a solid clue why some IBS patients end up with bright‑red spotting.
IBS‑Related Issues That Can Cause Bleeding
Hemorrhoids & Chronic Straining
When you’re fighting constipation, the pressure you exert to pass a hard stool can swell the veins in your rectum. Those swollen veins = hemorrhoids. In IBS‑C folks, the habit of “holding it in” and then “pushing like there’s no tomorrow” is a recipe for tiny ruptures that bleed.
The IBS Dietitian notes that hemorrhoids are “more common in people with IBS compared to the general population” (source).
Anal Fissures & Small Tears
On the flip side, IBS‑D (diarrhea‑predominant) can cause frequent, watery trips. The gut’s rapid contractions sometimes slap the anal lining, creating a fissure—a tiny cut that bleeds a little with each movement. These tears are often painful, but the bleed is usually bright red and easy to spot on toilet paper.
Inflammation & Mucus‑Related Irritation
IBS can crank up mucus production. During a flare, excess mucus can act like a slippery lubricant, but it also means the delicate lining gets a bit more exposed. Occasionally, that irritation leads to micro‑bleeds that show up as faint pink streaks.
Comparison Table – IBS‑D vs. IBS‑C Bleeding Risks
| Feature | IBS‑D (Diarrhea) | IBS‑C (Constipation) | Typical Blood Appearance |
|---|---|---|---|
| Common cause | Anal fissure, occasional hemorrhoid | Hemorrhoid, anal skin tear | Bright‑red, often on toilet paper |
| Frequency | Sporadic, linked to sudden loose stools | More frequent with straining episodes | Variable, depends on severity |
When to Take Blood Seriously
Red‑Flag Symptoms
Not all blood is created equal. If you notice any of these, it’s time to call a healthcare professional:
- Persistent bleeding for more than three weeks
- Severe abdominal pain or a palpable lump
- Weight loss, fever, or night sweats
- Black, tarry stool (possible upper‑GI bleed)
- Accompanying dizziness, weakness, or fainting
Quick Self‑Screen Checklist
Ask yourself these three questions:
- Is the blood bright red and only on the surface of the stool or toilet paper? → Likely a low‑down issue (hemorrhoid or fissure).
- Is the blood dark red, brown, or black? → Could be higher up (colon, stomach) – seek care.
- Are you experiencing other warning signs (pain, weight loss, anemia)? → Get evaluated ASAP.
What the Doctor Will Do
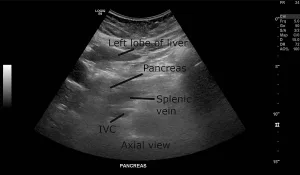
When you walk into the clinic, the doctor may order:
- A stool occult blood test – catches hidden bleeding.
- Colonoscopy – visualizes the colon and rectum.
- Blood work – checks for anemia or infection.
WebMD advises that any unexplained bleeding lasting more than three weeks or paired with severe symptoms should trigger a medical appointment (source).
Managing the Bleeding‑Risk Factors in IBS
Diet & Hydration Strategies
Fiber is your best friend, but not every fiber works the same. Soluble fiber (oats, apples, carrots) softens stool, while insoluble fiber (whole wheat, nuts) adds bulk. Aim for 25–30 g daily, and drink at least 8 cups of water. If you’re on a low‑FODMAP plan, work with a dietitian to keep the fiber steady without triggering gas.
Lifestyle Tweaks
Stress loves to hijack IBS. When anxiety spikes, the gut reacts—often with either a dash of diarrhea or a bout of constipation, both of which can lead to bleeding injuries. Incorporate:
- Mindful breathing or short meditation sessions (5 minutes, twice a day).
- Gentle yoga or a brisk 20‑minute walk after meals.
- Regular sleep schedule – your gut thrives on rhythm.
A 2024 article from the IBS Gut Health Clinic highlighted that stress reduction can lower the frequency of IBS‑related flare‑ups, which indirectly reduces the chance of hemorrhoids and fissures forming.
When Over‑the‑Counter Is Helpful
For occasional hemorrhoid discomfort, try:
- Topical witch‑hazel pads (cooling, astringent).
- Hydrocortisone creams (short‑term use only).
- Sitz baths – sit in warm water for 10 minutes after a bowel movement.
- Stool softeners (docusate sodium) if constipation is the main culprit.
Never rely on OTC solutions for weeks without checking in with a doctor; persistent bleeding could mask a more serious issue.
Sample 7‑Day Meal Plan (Optional)
Here’s a quick glance at a balanced, low‑FODMAP-friendly week that keeps fiber up and irritation down:
- Day 1: Oatmeal with strawberries, lactose‑free yogurt, and a handful of walnuts.
- Day 2: Grilled chicken, quinoa, steamed carrots, and a side of spinach.
- Day 3: Scrambled eggs, gluten‑free toast, and a banana.
- Day 4: Baked salmon, brown rice, and roasted zucchini.
- Day 5: Lentil soup (low‑FODMAP version), cucumber salad.
- Day 6: Turkey meatballs, gluten‑free pasta, tomato‑basil sauce (watch for nightshades if you’re sensitive).
- Day 7: Smoothie with kefir, blueberries, and chia seeds.
Pair each meal with a glass of water and a short walk afterward to help keep things moving.
Frequently Asked Questions (Featured‑Snippet Ready)
Can IBS cause blood in stool?
IBS itself doesn’t cause bleeding, but the constipation or diarrhea it brings can create conditions—like hemorrhoids or anal fissures—that do. So the answer is: “Indirectly, yes, in certain situations.”
What does bright‑red blood indicate?
Bright‑red blood usually means the source is low in the digestive tract: the rectum, anus, or just above. Common causes are hemorrhoids, fissures, or a small tear from straining.
Is black (tarry) stool an emergency?
Yes. Black, tarry stool (melena) suggests bleeding higher up, often from the stomach or duodenum. It warrants urgent medical evaluation.
How often can I see blood if I have IBS?
Occasional spotting after a hard bowel move can be normal for IBS‑C, but repeated or daily bleeding isn’t. If it happens more than a few times a month, get checked.
Does stress trigger bleeding in IBS?
Stress can intensify IBS symptoms—more diarrhea or tighter constipation—both of which increase the risk of hemorrhoids or fissures. Managing stress is a proactive way to lower bleeding chances.
Real‑World Perspectives (Experience)
Patient Story Snippet
Sarah, a 34‑year‑old graphic designer, lived with IBS‑C for five years. She’d often feel a “balloon” in her lower abdomen and would push hard to pass the occasional hard stool. One morning she noticed bright red specks on the toilet paper. A quick visit to her GP revealed a small external hemorrhoid. After adding fiber, drinking more water, and using a sitz bath, the bleeding stopped within two weeks. Sarah says, “I thought the blood meant something awful was happening, but it turned out to be a simple, fixable irritation.”
Professional Quote
Dr. Anita Patel, a board‑certified gastroenterologist, explains, “When a patient with IBS reports blood, our first step is to rule out serious conditions like IBD or colorectal cancer. If those are excluded, we look for secondary causes—hemorrhoids, fissures, or medication side‑effects.” She adds that regular follow‑ups are key because IBS can evolve over time.
Conclusion
Finding blood in your stool can feel like a red flag flashing in your mind, yet the reality is a bit more nuanced. Blood isn’t a hallmark of IBS, but the way IBS messes with your bowel habits can set the stage for low‑down injuries that bleed. Knowing the difference between a harmless hemorrhoid and a sign of something deeper empowers you to act wisely—use the quick self‑screen checklist, stay on top of diet and stress, and never hesitate to call your doctor when red‑flags appear.
If you’ve experienced any of the scenarios discussed, or if you have questions about your own gut health, drop a comment below. Sharing your story could help someone else feel less alone, and we’re all in this journey together.






















Leave a Reply
You must be logged in to post a comment.