Hey there, friend. If you’ve landed on this page you’re probably looking for clear, honest information about opioid use disorder (OUD) – maybe for yourself, a loved one, or just out of curiosity. I’m not a robot; I’m someone who’s sat with people at a coffee shop, listened to their worries, and watched the good news stories of folks getting back on their feet. So let’s have a real conversation about what OUD is, why stable housing matters, and how the right mix of treatment and support can make a world of difference.
What Is OUD
First things first: opioid use disorder is a medical condition, not a moral failing. In plain language, it means a person’s brain and behavior have been changed by repeated opioid use to the point where they keep using despite negative consequences. The CDC says that a formal diagnosis follows the DSM‑5 checklist – at least two of eleven criteria within a year. The more criteria you meet, the more severe the disorder (mild, moderate, severe).
It’s easy to confuse physical dependence (your body gets used to a drug and shows withdrawal) with OUD (which adds compulsive cravings, loss of control, and life‑disrupting patterns). Think of it like this: dependence is the “engine” that keeps running, while OUD is the driver who refuses to stop even when the road is clearly headed for a crash.
Who’s at risk? Anyone who’s taken opioids for 90 days or more, whether it was a prescription after surgery or a chronic pain regimen. Genetics, mental‑health challenges, and stressful life events also raise the odds. In the United States, about 6 million people are living with OUD – that’s roughly the entire population of a midsize city.
Why Housing Matters
Imagine trying to quit smoking while living on a park bench. It’s a harsh image, but it mirrors the reality for many people with OUD who are also experiencing homelessness. Unstable housing amplifies stress, triggers cravings, and makes it harder to stick with medication‑assisted treatment (MAT). Conversely, stable housing can be a powerful therapeutic tool.
Research shows that people who receive “Housing First” – immediate, permanent housing without pre‑conditioned sobriety requirements – have lower emergency‑room visits and higher treatment retention. A 2023 study in Lancet Public Health found that participants in a supportive‑housing‑plus‑MAT program had a 45 % reduction in overdose deaths compared with those who remained unhoused.
When you look at the bigger picture, the costs of untreated OUD (hospitalizations, law‑enforcement, lost productivity) dwarf the investment needed for stable housing. In other words, paying for public health housing actually saves money – a win‑win for communities and individuals.
Effective Treatments
Now let’s dive into the good news: OUD is treatable, and there are several evidence‑based options that work together like a well‑orchestrated band.
Medication‑Assisted Treatment (MAT)
MAT combines FDA‑approved medicines with counseling and behavioral support. The three main medications are:
- Methadone – a long‑acting opioid agonist that reduces cravings and blocks withdrawal.
- Buprenorphine – a partial agonist that offers a “ceiling effect,” meaning the high‑risk of overdose is much lower.
- Naltrexone – an opioid antagonist that blocks the euphoric effects of any opioid you might take.
A 2024 article in JAMA reported that MAT cuts overdose mortality by about 50 %. Dr. Volkow of the National Institute on Drug Abuse (NIDA) calls MAT “the gold standard” for OUD care.
Therapy & Counseling
Medication alone isn’t a magic bullet. Cognitive‑behavioral therapy (CBT), motivational interviewing, and peer‑support groups help reshape thoughts, manage triggers, and rebuild social connections. Many programs blend weekly counseling with daily medication dosing.
Housing‑Integrated Care
This is where the magic of “housing hope” really shines. Programs that pair MAT with supportive housing (think on‑site case managers, easy access to doctors, and a safe place to sleep) see higher retention rates. A participant from Seattle shared, “I finally felt like I owned a piece of my life again when I had a key in my pocket and a nurse I could call at 2 a.m.”
Linking Housing & Care
Let’s break down how you can turn the abstract idea of “supportive housing” into concrete steps.
What Is Supportive Housing?
Supportive housing provides affordable, stable homes plus on‑site services such as medical visits, counseling, and life‑skills training. It’s not a shelter; it’s a home with a safety net.
Cost‑Effective Solutions
Many cities are leveraging “cost‑effective housing solutions” by repurposing vacant apartments, using low‑income tax credits, and partnering with nonprofit developers. The upfront cost per unit may seem high, but the downstream savings in emergency care and incarceration are massive. Cost‑effective housing solutions often pay for themselves within five years.
Homelessness Prevention Programs
Prevention is better than cure. Programs that intervene before a person loses their home – offering rent assistance, legal aid, or rapid re‑entry services – dramatically lower the odds of relapse. Check out the homelessness prevention programs page for real‑world examples.
Step‑by‑Step Checklist
| Step | What to Do |
|---|---|
| 1. Confirm Diagnosis | Visit a clinician, complete the DSM‑5 checklist (CDC guidelines). |
| 2. Explore MAT Options | Ask about methadone, buprenorphine, or naltrexone; discuss insurance coverage. |
| 3. Locate Housing Resources | Contact local HUD office, community nonprofits, or your state’s public health housing portal. |
| 4. Apply for Integrated Programs | Look for “Housing First + MAT” projects; many accept referrals from doctors. |
| 5. Build a Support Network | Engage family, peer groups, and case managers; keep a list of emergency contacts. |
Each of these steps is a brick in the foundation of lasting recovery. It may feel overwhelming, but remember: you don’t have to lay every brick yourself. Professionals, advocates, and even friends (like me) are here to hand you a few at a time.
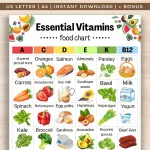
Everyday Strategies
Beyond the big‑picture treatment plan, there are daily habits that can keep you or your loved one steady on the path to health.
- Keep Naloxone Handy – One dose can reverse an overdose in minutes. Many pharmacies now dispense it without a prescription.
- Use Test Strips – Fentanyl test strips can spot hidden potency in “street” pills.
- Stay Connected – A quick text to a trusted friend or a check‑in call can break a crisis loop.
- Mind‑Body Practices – Simple breathing exercises, walking, or journaling can lower stress that often triggers cravings.
- Access Free Resources – The CDC offers a free “Overdose Prevention” guide; many states have 24‑hour hotlines.
One of my colleagues, a recovery coach, swears by a “morning checklist”: medication taken, appointment confirmed, support person pinged, and a small win recorded (like making the bed). Small wins add up to big victories.
Myths Debunked
Let’s smash a few lingering misconceptions that keep people stuck.
Myth 1: “Only “hard” drug users get OUD.”
False. Most people start with a legitimate prescription for pain. The risk climbs after 90 days of use, regardless of the drug’s legality.
Myth 2: “MAT is just swapping one drug for another.”
Not true. Medications like buprenorphine have a ceiling effect that prevents dangerous respiratory depression. Studies repeatedly show MAT reduces overdose deaths and improves quality of life.
Myth 3: “If you’re in treatment you can’t work.”
Many people on MAT hold steady jobs, attend school, and raise families. The stability that medication provides often makes employment possible.
Myth 4: “Supportive housing is only for “addicts” on the streets.”
Supportive housing is a public‑health tool for anyone whose medical condition (including OUD) makes stable housing difficult. It’s about dignity, not stigma.
Conclusion
Opioid use disorder is a tough beast, but it’s not unbeatable. The science tells us that medication, counseling, and stable, supportive housing form a three‑legged stool that can hold up a life of recovery. By understanding the condition, tapping into cost‑effective housing options, and leaning on compassionate professionals, you—or someone you care about—can rewrite the story from “trapped” to “thriving.”
If you feel ready to take the next step, start with a simple conversation: call your doctor, reach out to a local supportive housing homelessness resource, or explore homelessness prevention programs in your area. You don’t have to walk this path alone. Together, we can turn hope into a home, and a home into lasting health.





















Leave a Reply
You must be logged in to post a comment.