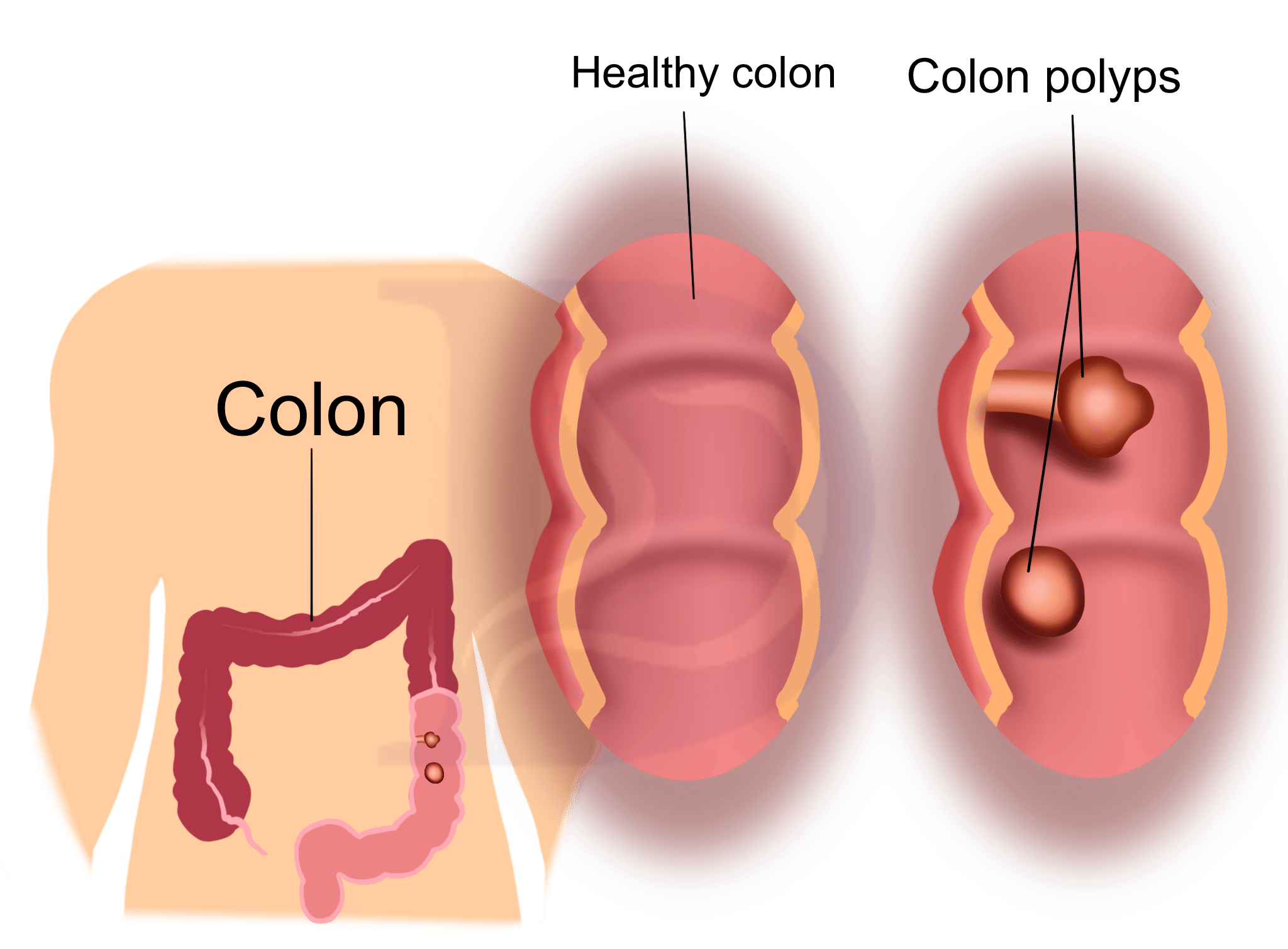
Polyps are tissue overgrowths that usually appear as tiny, flat nodules or small stalked projections resembling mushrooms. They are commonly small, typically under half an inch in diameter. While most are noncancerous, some can progress to cancer.
Uterine and colon polyps are the most frequently seen, but polyps can also form in areas such as the:
- ear canal
- cervix
- stomach
- nose
- throat
The majority of polyps are benign, meaning they are not cancerous. However, because they represent abnormal cell growth, they have the potential to become malignant over time.
Your healthcare provider can determine whether a growth is a polyp by performing a biopsy, which involves removing a small tissue sample to test for cancerous cells.
Treatment for polyps is guided by factors such as:
- their anatomical location
- their size
- whether they are benign or malignant
Read more about colonic polyps and colon cancer.

What are the symptoms of polyps?
Symptoms vary by polyp type and where it forms. Below are common polyp varieties, where they occur, and typical symptoms.
| Type of polyps | Location | Symptoms |
| colorectal (colon) | large intestine, colon, and rectum | blood in the stool, abdominal discomfort, constipation, diarrhea |
| endometrial (uterine) | uterus, frequently the uterine lining | infertility, irregular menstrual bleeding, vaginal bleeding |
| cervical | cervix, where the uterus meets the vagina | often asymptomatic, but may cause heavier menstrual bleeding, bleeding after sex, or unusual discharge |
| gastric (stomach) | stomach and stomach lining | nausea, abdominal pain, tenderness, vomiting, bleeding |
| nasal | nose or near the sinuses | symptoms like a common cold: headache, nasal pain, reduced sense of smell |
| aural | ear canal | hearing loss and blood drainage from the ear |
| vocal cord (throat) | vocal cords | a hoarse or breathy voice that develops over days to weeks |
| bladder | bladder lining | blood in the urine, painful urination, frequent urination |
| gallbladder | gallbladder lining | right-sided abdominal pain, bloating, nausea, difficulty eating |
Most colon polyps are benign and frequently remain symptom-free until later stages. However, like stomach polyps, they can progress to cancer. Up to 13 percent of endometrial polyps may also become malignant.
What causes polyps?
The origins of polyps differ depending on their site.
Research indicates that certain genetic alterations or a family history of hereditary syndromes can increase the likelihood of developing specific polyp types. Lynch syndrome (hereditary non-polyposis colorectal cancer, HNPCC) is one such example.
Some established causes include:
- inflammation
- presence of a foreign body
- a cyst
- a tumor
- mutations in colon cell genes
- genetic predisposition or hereditary syndromes
- chronic stomach inflammation
- excess estrogen
While some polyps arise from identifiable reasons, others develop without a clear cause.
Below are specific reasons linked to certain polyp types.
Colon polyps
Colon polyps form when the mucosal lining of the colon undergoes changes. They may appear sporadically with no obvious cause, or due to genetic changes or conditions like inflammatory bowel disease (IBD).
Uterine polyps
Endometrial polyps develop within the uterus when portions of the endometrial glands enlarge and project from the endometrial lining. The exact reason is uncertain, but elevated estrogen levels seem to play a role.
Cervical polyps
The precise cause of cervical polyps is unknown, but possible contributors include:
- congestion of cervical blood vessels, disrupting blood flow and encouraging polyp formation
- infection or chronic cervical inflammation
- long-term exposure to irritating chemicals
- elevated estrogen levels
Throat polyps
Factors that can lead to throat polyps include:
- vocal trauma from loud shouting
- damage from gastroesophageal reflux
- smoking
- intense respiratory strain
- exposure to irritating chemicals
Nasal polyps
Nasal polyps are commonly triggered by inflammation, which may result from fungal or bacterial infections or allergic reactions. They can also be associated with conditions like cystic fibrosis or refractory nasal polyposis affecting the sinuses.
Polyps expand because of rapidly dividing cells, a process similar to how cancer cells grow. This is why they can sometimes turn cancerous, even though most are benign.
What are the risk factors of polyps?
People who frequently strain their vocal cords or have acid reflux are at greater risk for throat polyps. There are no well-established risk factors for aural polyps.
Men and smokers are at increased risk for bladder polyps. Bladder polyps are uncommon, and the exact reasons are not well understood. The bladder’s nicotine receptors may make bladder cells more susceptible to change, increasing cancer risk from smoking changes.
If you’re worried about your risk for a particular polyp type, discuss it with your doctor.
Risks for colon polyps
Risk factors for colon polyps include:
- certain genetic traits
- having a hereditary condition, such as familial adenomatous polyposis or Lynch syndrome
- a high-fat, low-fiber diet
- older age—about 30 percent of U.S. cases occur in people over 50
- male sex
- a family history of colon polyps or colon cancer
- use of tobacco or alcohol
- intestinal inflammatory disorders like IBD
A 2015 study found Black people develop polyps earlier than white people and suggested screening begin at 45 rather than 50. Black Americans also face a higher rate of colorectal cancer mortality, with a 35 percent greater chance of death compared with white Americans, per a 2018 article in The American Journal of Pathology.
Further research is needed to understand these disparities, though socioeconomic factors likely contribute. Earlier screening could help reduce risk since some polyps can transform into cancer.
Risks for stomach polyps
The likelihood of stomach polyps increases with:
- advancing age
- chronic inflammation or irritation where polyps form
- bacterial infections of the stomach
- familial adenomatous polyposis (FAP)
- regular use of proton pump inhibitors (e.g., Nexium, Prilosec, Protonix)
Risks for uterine polyps
You are more likely to be diagnosed with uterine or endometrial polyps if you:
- are older than 60
- have elevated estrogen levels
- have gone through menopause
- experience symptoms such as bleeding
- have polycystic ovarian syndrome
- have a history of long-term tamoxifen use
Risks for cervical polyps
You are more likely to develop cervical polyps if you:
- have not reached menopause
- have been pregnant one or more times (multigravida)
- have a sexually transmitted infection
- have had cervical polyps previously
Risks for nasal polyps
Nasal polyps are more common in people with:
- chronic sinus infections
- allergies
- asthma
- cystic fibrosis
- aspirin sensitivity
Risks for vocal cord polyps
You may be more likely to develop vocal cord polyps if you:
- overuse or strain your voice
- have sulcus vocalis (a groove on the vocal cord)
- smoke
- are exposed to certain chemicals
- suffer from acid reflux
Gallbladder polyps
Experts are uncertain about gallbladder polyp risk factors, but you may be more prone to them if you:
- have a family history of gallbladder polyps
- have Peutz-Jeghers or Gardner syndrome
- have hepatitis B
- have repeated inflammation from cholecystitis or biliary colic
High cholesterol or bile salt levels can lead to cholesterol deposits on the gallbladder wall that look like polyps but are actually clumps of cholesterol. These so-called cholesterol or pseudopolyps account for 60 to 90 percent of polyp-like structures in the gallbladder.
Risks for bladder polyps
You may have a higher risk of bladder polyps if you are male and smoke tobacco.
How are polyps diagnosed?
Your provider will conduct a physical exam and review your symptoms and medical history.
If polyps are suspected, imaging such as X-rays, ultrasound, or CT scans may be used to visualize the area and estimate the size and presence of polyps.
The diagnostic approach depends on the polyp’s location. Methods for sampling tissue include:
- esophagogastroduodenoscopy (endoscopy) for the stomach and small intestine
- biopsy of easily reachable areas for microscopic analysis
- colonoscopy for polyps in the colon
- visual inspection of the throat with a mirror to check the vocal cords
- nasal endoscopy to examine the nasal cavity
In some instances, a biopsy is performed to determine whether the polyp is cancerous.
What are the risks of a polyp biopsy?
How are polyps treated?
Treatment varies widely depending on polyp type and location. In many cases, clinicians remove polyps.
Some polyps do not require treatment because they pose little risk. Throat polyps often resolve with rest and voice therapy. Doctors may surgically remove polyps as a precaution to reduce the chance of future cancer.
Factors that influence treatment include:
- the likelihood the polyps are cancerous
- the number of polyps
- their location
- their size
For colorectal polyps, physicians typically remove them during colonoscopy because appearance alone cannot confirm cancer risk.
A colonoscopy involves using a flexible tube with a camera to inspect the rectum and large intestine. Routine screening colonoscopies are advised because they can detect and remove polyps before cancer develops.
Hormone-related polyps such as cervical and uterine polyps may be treated with progestin or gonadotropin-releasing hormone agonists. These medications alter hormone signaling to shrink or reduce the polyps.
Nasal steroids or other corticosteroid treatments may help with nasal polyps.
Doctors usually choose the least invasive option before recommending surgery.
Here, find out more about removing uterine polyps.
How are polyps prevented?
Preventing all polyps is not always possible, but avoiding certain risk factors may lower the chance of some types.
Awareness of risk factors can help reduce the likelihood of developing polyps like colon polyps, which in turn may lower colorectal cancer risk.
Preventive measures include:
- asking your doctor about routine screening colonoscopy
- eating a nutrient-rich diet with plenty of fruits, vegetables, and whole grains
- limiting alcohol intake
- avoiding tobacco
- exercising regularly to maintain a healthy weight
Discuss additional preventive steps with your physician, particularly if you have a family history of polyps.
What are the next steps for someone with polyps?
Asymptomatic, noncancerous polyps often don’t need immediate treatment unless they interfere with daily life. Your doctor may recommend watchful waiting—monitoring the polyps to ensure they do not progress. They will advise if and when surgical removal is necessary.
If you’re concerned about polyps, you can:
- learn more about your family history of polyps and discuss it with your doctor
- keep records of prior tests and imaging related to your diagnosis
- follow up with your physician after polyp removal to confirm you are clear
- be alert to polyp symptoms and seek care when they occur
Colon polyps require increased monitoring, such as more frequent colonoscopies. Talk with your provider about how often you should be screened. Screening intervals depend on:
- the polyp type
- how many polyps are present
- family history
What is the outlook for someone with polyps?
Your clinician will review the prognosis for your particular situation. The outlook varies based on:
- the polyp type
- whether they are cancerous
- your overall health
Most benign polyps are unlikely to cause long-term problems, but doctors may remove them as a preventive measure.
Benign polyps can sometimes become malignant or cause symptoms that affect quality of life. Uterine polyps may impact fertility, and nasal polyps can cause persistent nasal congestion.
Colon polyps can indicate an increased risk of colorectal cancer.
For example, a solitary 1-centimeter colon polyp that develops without a clear reason has about an 8 percent chance of becoming cancerous after 10 years and a 24 percent chance after 20 years. It’s important to follow your doctor’s guidance about follow-up for colon and other potentially precancerous polyps.
Summary
Polyps can arise in various body regions, including the colon, uterus, nose, and ears. While most are harmless, some can transform into cancer over time.
If you notice signs of polyps or experience symptoms such as rectal or vaginal bleeding, seek medical evaluation.


















Leave a Reply
You must be logged in to post a comment.