Ever noticed how sometimes ongoing symptoms feel like they’re being ignored by your doctor? If you’re in your 60s or older and dealing with relentless watery diarrhea, your concerns are valid. The term “microscopic colitis” might come up in conversations, and here’s the fast truth? There’s no clear evidence that your medications are triggering this. Whether you’re scrolling late-night, worried about your health, or your doctor mentioned MC for the first time, we’re here to talk plainly — no long-winded medical speak, no academic dryness. Just clear, helpful info from someone who understands this condition isn’t easy thing to live with.
“Wait… if not medications, then what the heck is happening? — you ask. That’s fair. Let’s cut through the fluff, the half-answered Google searches, the vague ‘if’ and ‘maybe’ that drive us bonkers. Microscopic colitis matters — especially if it’s disrupting your daily life, making you think twice before stepping out, or explaining ‘those’ moments that come out of nowhere. This isn’t about jumping to conclusions… it’s about digging into what we do know and finding pathways back to control without unnecessary fear about the drugs we rely on.”
Understanding Microscopic Colitis
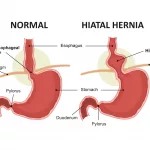
Let’s start at the beginning — but not the typical academic version. Imagine this: you’re dealing with unexplained, constant watery stool, the kind that doesn’t scream emergency but is stubborn. You try everything — hydration, laxatives nothing works. Then finally, someone says one of those vague, unhelpful doctor phrases like “just old age” or “maybe IBS.” Wrong. Welcome to microscopic colitis territory, the disease no one hears about until it attacks your rhythm and your toilet schedule.
So what even is microscopic colitis?
MC basics: It’s stubborn, sneaky and lives only under the microscope
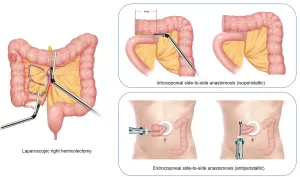
Making it simple: microscopic colitis is chronic inflammation of the colon, but it hides in plain sight. Standard colonoscopies show a normal intestine. No visible damage, no blood in stool. But when a gut doctor takes a tissue sample under the scope, and slides it under the microscope, out pops the inflammation — and there you have your diagnosis.
What are the types, and which one’s worse?
Three MC forms that can affect the elderly: collagenous, lymphocytic, mastocytic
There are at least a dozen known types, but these three pop up most often:
| Collagenous Colitis | Lymphocytic Colitis | Mastocytic Enterocolitis |
|---|---|---|
| Thick collagen band (over 10μm) beneath cells lining your gut — common in post-menopausal women. | High levels of white blood cells (lymphocytes) inside that same lining — mostly affecting women slightly younger than those with collagenous colitis. | Mast cells (think allergy alarm) gone crazy in your intestines — linked to higher symptom variability. Some older adults feel like they’ve been dealing with low-grade flu that won’t quit. |
One thing important to mention – you don’t need to fixate on which one you have. Most experts treat all three similarly on a symptom-guided approach. Like cracked walls in a house: whether it’s concrete or brick, the solution is often still patch and stabilize first, question layout later.
Medication Fears: Debunking the Rumors Out There
“Wait, my doctor asked if I’m taking anything new. Could my blood pressure pills be behind this?” Many seniors worry their meds are toxic. And for valid reasons — drugs are tough. But stick with me here,
“But my meds make my stomach feel weird” — is that a red flag for MC?
Four meds often discussed, and whether they’re likely culprits
Here’s the real breakdown, cross-checked with Crohn’s & Colitis Foundation and NIDDK:
- NSAIDs (like ibuprofen or naproxen): could irritate, but not proven to cause MC — especially not in older adults.
- Antidepressants (SSRIs like sertraline or paroxetine): Pop up in some MC studies. But correlation isn’t cause — not at this point anyway.
- Proton pump inhibitors (PPIs like omeprazole): Linked to MC in what we call “risk associations,” but the evidence isn’t rock-hard yet.
- Clozapine and entacapone: Rarely, but some case reports point suspicion here. Don’t panic — but discuss with your doctor if you’re on them.
The hotter this topic gets, the more patients tell countless versions. Maybe you’ve heard one elderly neighbor got worse after starting a new pill. That’s relatable. That’s human. But again, the medical evidence doesn’t quite call it a drug-triggered condition yet — not in older adults, at least. More on this later — specifically in the “what the studies say” section.
More Than Just the Runs: MC’s Hidden Impact on the Elderly
Microscopic colitis might sound like a fecal factory issue — and in a way, it is. But reduce this to “just watery poops” and you’re missing an entire chapter of silent chaos. Let’s be clear — we’re not downplaying this. For seniors, frequent diarrhea isn’t “cute.” It can be isolating. Planning dinners is risky. Live music outings or visiting an elderly parent mean calculating. What if it happens mid-conversation? Mid-car ride? That fear of faecal incontinence is a real parça of the MC midlife crisis. And for some, it’s not even about the toilet — it’s about fatigue, brain fog, and that dreaded nighttime run to the bathroom.
Wait, MC doesn’t just stop at diarrhea?”
Three worst MC symptoms no one warns you about
We’re familiar with watery diarrhea. The shock comes from what else it can bring — symptoms that feel like a sidekick from a toxic relationship:
- Nighttime diarrhea attacks. You lie down, thinking you’re finally safe — then you aren’t.
- Fear of public embarrassment. It sounds dramatic, but it’s a daily living hack for those with more than four trips a day.
- Severe fatigue – worse than “older adult sleep routine.” Because nobody rests well when they’re sprinting to the loo thrice before coffee.
And some seniors think it’s constipation mixed with erratic gut behavior — inflammation messes with gut movement timing, and your body isn’t a flexible puppy anymore. Keep an eye out for those hidden signs. They matter more than we’re sometimes told.
What Does Science Actually Say About MC Causes?
Here’s the thing with medical research: even if it isn’t tied to your pill bottle, sometimes it feels personal when you’re in pain. The microscopic colitis foundation acknowledges people in their community share countless stories of when symptoms flared — and what they isolated as the likely cause. One guy said it started after a bad stomach flu. Another mentioned increased gluten sensitivity before MC hit. So what do the big picture studies say?
“I had one flare pillar-to-post — is it infection-triggered MC?”
Infection, virus, or bacteria – a common trigger for MC
Researchers from BADGUT.org suggest that C. diff infections, food poisoning episodes, and even viral gut upsets (hello, norovirus) could in theory prime your colon for inflammation. So if you had a gut bug that just wouldn’t quit, and diarrhea shadowed you weeks after, that could be MC territory.
But also worth looking into: adult autoimmune conditions. If you’re already managing Hashimoto’s thyroiditis, Celiac, or Rheumatoid arthritis, microscopic colitis fits in that cluster — not fixed, not predictable, but related.
“I thought I was going into IBS panic — turns out it’s MC? How’s that possible?”
Why doctors confuse IBS and MC — and what happens when it takes forever to diagnose
Here’s a harsh fact: microscopic colitis is often misdiagnosed as IBS (Irritable Bowel Syndrome) — and it cuts across all patient groups, especially older patients. Part of the issue is the colon lining looks pristine on a colonoscopy — no inner volcanoes erupting, no storage of fire. That leads to rushed conclusions. Docs might skip the biopsy step — a standard practice that should be dive-in zone for chronic watery diarrhea in older adults. And the end result? You wait longer than you should to find the right path.
If you’re feeling surprised, like “No, my doctor definitely took biopsies?” then you hit the superhero half-minute — because you found your way to a gastro who gets it. But if not? Push for the biopsy next time. It might save months of IBS talk that was never accurate.
Living & Treating With MC: Real Options for Real Human Bodies
A lot of this disease boils down to one phrase we hear from seasoned MC patients: “I waited until it got unmanageable… and then we just detoxed it through lifestyle and pushed meds when needed.” That flexibility? It works. But here’s the non-sugarcoated version you’ve been aching for.
What’s the deal with the “gold standard” MC treatment – budesonide?
Breakdown of budesonide: How effective it is, side effects, and how long it lasts
Lucky news: we have a medical darling. Budesonide — the corticosteroid that sits on your colon, stays just strong enough to control inflammation, but doesn’t yank your immune system every which way. Studies from the 2024 Mayo Clinic window confirm that 80-90% of patients respond well, including the elderly ones and those with long-term prescription lists. The best part? It’s not the typical high-dose steroids most seniors fear — it’s low absorption, direct delivery in the gut tissue.
Don’t know where to start? Lifestyle changes that help — even without scripts
Eating, hydration, and quality of life hacks that actually work for MC
Before we dive into drug shelves, how do you usually adjust to MC without crushing anxiety? A few non-prescription lifelines pulled from “good stranger” blogs online:
- Hydration hacks – because adults forget they still need water.
- Gentle eating – ditch the five-star spicy challenge for MC-friendly staple meals (think oatmeal, rice, steamed veg).
- Stress management cards – not the warm-and-fluffy yoga aphorisms, but the serious kind: meditation, sleep support, and passtime relaxation because overactive stress hormones can press symptom buttons.
- You don’t have to be scared of usual drugs. More studies point elsewhere. Medications may blur symptoms — but they aren’t the guaranteed MC gateway.
- MC creeps up silently — colonoscopies sometimes miss, unless they tug texture from the inside. Pathologists spot it, gastro hustle gets you there faster.
- The elderly don’t have to suffer in silence. Night flares, fatigue, loss of confidence in leaving for dinner? Those are a real deal, and they deserve official diagnosis, not passing it off as “just what happens over 65.”
- Budesonide is your major intervention support — but also, hydration, meals, and lifestyle shifts create the win / lose scenario, especially when under control.
Real Talk: Meet Marie. Her MC Story Could Be Yours
Marie turned 68 — and suddenly, her tight digestion schedule became unpredictable. It wasn’t “hurried” — it was full-on beginning-and-end-of-the-day intervention mode. She tried over-the-counter meds, talked to two doctors, and got an “IBS is just living old” diagnosis. Until one junior doc asked three simple questions that changed everything: how long’s this been going on? Any new meds or habits? And had you slept well before this started?
So what finally helped Marie and how she told it
Marie’s MC lifeline: design of the current road to stability
Her specific aha moments? For starters — going on the peel protocol: higher hydration with electrolytes, reduced caffeine and processed sugars. And even though she plays all-in on gluten & dairy-free living, she realized it wasn’t enough for extended remission. So, budesonide was introduced. Eight weeks in? She felt like herself again — and after twelve, she asked her doctor about long-term meds. Turns out budesonide’s not an everyday use pill for MC, but when you have flares, it’s the big red stop knob.
Side kicker to her story: she kept tobacco. Some studies point out smoking increases relapse risk for MC patients — and while she was a moderate smoker, cutting back was a suggestion she took seriously. “I didn’t stop overnight,” she told us, “but even slowing down helped with everything — digestion, anxiety, and those resource-hungry elderly health expenses.”
Taking Back Control: The Real Final Word
If you’re reading this and thinking, “I’m not imagining this gut issue,” good. If you’re nodding along and imagining a “what’s next” plan for your MC-like symptoms, we’re halfway there.
Here’s the very digestible summary:
A question: are there still unresolved feelings around possible triggers and symptoms? If this is the start to MC self-discovery, take a deep breath. This isn’t untreatable. It isn’t a one-way ticket to feeling worse. Work with your gut, reshape your environment, and stay open with your specialist. But don’t let symptoms anchor you to the bathroom — start the conversation. Dive into what’s affecting you and stop guessing.
Microscopic colitis isn’t just your pills, your “weaker old metabolism” — it’s a real low-key digestive condition that deserves proper care. Take the next step. Help yourself — small biopsies, small treatment shifts, and small victories matter more than massive medical overhauls. If you want to check the technical references, including the full MC patient findings from the Microscopic Colitis Foundation — feel free to dive in later. But for now? Keep your confidence, grab your cholestyramine sample, and keep your favorite herbal teas without jumping to alternative solutions. You’re stronger than a condition that hides under the microscope — prove it by managing it your way.























Leave a Reply
You must be logged in to post a comment.