Regular physical activity, stress management, and eating more fiber- and probiotic-rich foods can help reduce blood glucose. Still, these lifestyle steps don’t replace prescribed medical care for diabetes or other metabolic disorders.
Your body normally controls blood glucose by releasing insulin, which enables cells to absorb circulating sugar. Yet various factors can disrupt glucose control and cause hyperglycemia (elevated blood sugar).
Keeping blood sugar in check is particularly vital for people with diabetes, since poor control can lead to limb-threatening and life-threatening complications.
Below are 14 practical, research-supported strategies to help naturally lower blood glucose.

Move and exercise throughout the day
Consistent exercise and staying active help with weight control and improve insulin sensitivity — meaning your cells use blood glucose more effectively.
Physical activity also enables muscle tissue to use blood sugar for energy and contraction.
If you struggle with glucose control, consider checking your levels regularly before and after workouts. This helps you understand how different activities affect your glucose and prevents excessive highs or lows.
Even short bursts of activity are helpful if you can’t fit long sessions into your schedule. Aim for three 10-minute sessions per day on most days to reach about 150 minutes weekly.
“Exercise snacks” — brief breaks from sitting every 30 minutes — also reduce the harms of prolonged sitting. Examples include light walking or simple resistance moves like squats or leg lifts.
Other effective activities include:
- weight training
- brisk walking
- running
- cycling
- dancing
- hiking
- swimming
- jumping jacks
- partial squats
Any movement that gets you off the couch — regardless of intensity — is preferable to remaining sedentary.
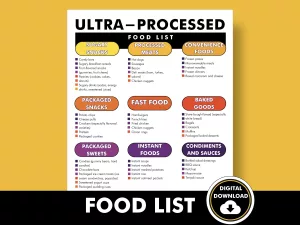
Control carbohydrate intake
Carbohydrates have a strong influence on blood glucose. The body breaks carbs into sugars (mainly glucose), and insulin helps cells use and store that glucose for energy.
When you consume too many carbs or insulin function is impaired, blood glucose can rise.
That’s why the American Diabetes Association advises people with diabetes to monitor carbohydrate intake by counting carbs and understanding how many are appropriate for daily needs.
Carb counting helps you plan meals to support better glucose control.
Lower-carb diets can reduce blood sugar and blunt large post-meal spikes.
Note that “low-carb” and “no-carb” diets are not the same.
You still need some carbohydrates, but prioritizing whole, unprocessed carbohydrate sources offers more nutrients while helping control blood sugar.
Increase fiber intake
Fiber delays the digestion of carbohydrates and slows sugar absorption, causing a gentler rise in blood glucose.
There are two main fiber types: insoluble and soluble.
Both matter for overall health, but soluble fiber has been linked to improved blood sugar control, whereas insoluble fiber has not shown the same effect.
A fiber-rich diet can enhance your body’s ability to modulate and reduce blood glucose. This may also aid in managing type 1 diabetes better.
Foods high in fiber include:
- vegetables
- fruits
- legumes
- whole grains
General recommendations are about 25 grams per day for women and 35 grams for men — roughly 14 grams per 1,000 calories consumed.
Stay hydrated
Drinking sufficient water may help keep blood glucose within a healthy range. Besides preventing dehydration, water assists the kidneys in excreting extra sugar via urine.
An analysis of observational studies found that higher water intake was associated with a lower risk of developing high blood sugar.
Regular water consumption may rehydrate blood, lower glucose, and reduce diabetes risk.
Water and other zero-calorie drinks are best for hydration. Avoid sugar-sweetened beverages, which raise blood glucose, contribute to weight gain, and increase diabetes risk.
Use portion control
Controlling how much you eat helps manage calorie intake and maintain a healthy weight.
Weight management supports healthy blood sugar and has been shown to lower the chance of developing type 2 diabetes.
Watching portion sizes can also prevent blood sugar surges.
Ways to control portions include:
- eating slowly
- measuring or weighing food
- using smaller plates
- avoiding buffets or restaurants with very large servings
- reading nutrition labels to check serving sizes
- keeping a food log
- using a food-tracking app
Pick low-glycemic foods
The glycemic index (GI) indicates how quickly carbohydrates are digested and absorbed, which affects how fast blood sugar rises.
Foods are scored from 0 to 100 and categorized as low, medium, or high GI. Low-GI foods have lower scores. Regularly choosing low-GI items may help lower blood glucose in people with diabetes.
Examples of low-to-moderate GI foods include:
- bulgur
- barley
- unsweetened Greek yogurt
- oats
- beans
- lentils
- legumes
- whole wheat pasta
- non-starchy vegetables
Adding protein or healthy fats to meals also helps reduce post-meal glucose spikes.
Focusing on overall food quality is more effective than cutting or adding isolated food groups.
Reduce stress
Stress can impact blood glucose. During stress, the body releases hormones such as glucagon and cortisol, which raise blood sugar.
Stress-reduction techniques may include:
- exercise
- meditation
- mindfulness
- deep breathing
- journaling
- arts and crafts
- psychotherapy
- enjoyable hobbies
Relaxation practices and physical activity may also help normalize insulin secretion in people with chronic diabetes who are receiving treatment.
Monitor your blood glucose
Tracking blood glucose helps you manage it. You can measure levels at home with a portable glucometer if recommended by your healthcare provider.
Recording readings helps you decide whether to alter meals or medications and teaches you how your body reacts to particular foods.
Try logging daily readings and measuring paired values — for example, before and after exercise or before and two hours after eating.
This approach can reveal whether small meal adjustments (like swapping a starchy side for non-starchy vegetables or limiting portion size) can prevent spikes instead of eliminating favorite dishes entirely. For people interested in alternatives to finger-stick testing, a diabetes blood sugar monitor without finger pricks may be worth discussing with a clinician.
Prioritize quality sleep
Poor sleep and inadequate rest can impair blood glucose control and insulin sensitivity, raising the risk of type 2 diabetes. They can also increase appetite and lead to weight gain.
Sleep loss raises cortisol levels, which play a key role in glucose regulation.
Adequate sleep involves both duration and quality. Adults are generally advised to aim for 7–9 hours of good-quality sleep nightly.
To improve sleep:
- keep a regular sleep schedule
- avoid caffeine and alcohol near bedtime
- stay active during the day
- cut down on screens before bed
- keep your bedroom cool and comfortable
- limit daytime naps
- use calming scents like lavender
- avoid working or studying in bed if possible
- take a warm bath or shower before bed
- try meditation or guided imagery
Eat foods high in chromium and magnesium
High blood sugar and diabetes have been linked to micronutrient shortfalls, including chromium and magnesium.
Chromium plays a role in carbohydrate and fat metabolism and may enhance insulin action, supporting glucose control.
Foods with chromium include:
- beef, chicken, and turkey
- whole grains like barley
- produce such as green beans and apples
- almonds
However, the exact mechanisms behind these associations aren’t fully understood, and further research is required.
Magnesium also supports blood glucose regulation. Diets rich in magnesium are associated with a substantially lower diabetes risk.
Low magnesium may lead to insulin resistance and poorer glucose tolerance in people with diabetes.
If your diet already supplies ample magnesium and your blood levels are sufficient, supplements are unlikely to help.
Magnesium-rich foods include:
- dark leafy greens
- squash and pumpkin seeds
- tuna
- whole grains
- dark chocolate
- bananas
- avocados
- beans
Be cautious with so-called “medicinal” foods
Many foods and plants are promoted for medicinal benefits. However, evidence is limited because human studies are few or small, so firm recommendations are difficult.
Some foods claimed to lower blood glucose include:
- Apple cider vinegar: A review suggests this ingredient may lower blood glucose by slowing gastric emptying after meals. An animal study also showed reduced glucose spikes with apple cider vinegar, and the authors proposed it might help prevent metabolic issues in high-calorie diets.
- Cinnamon: This spice may lower blood glucose by improving insulin sensitivity and slowing carbohydrate digestion, which tempers post-meal glucose rises. More research is needed.
- Berberine: Preliminary evidence indicates berberine may reduce blood glucose by activating enzymes that break down glucose, enhancing tissue glucose uptake, and boosting insulin production. Additional studies are required.
- Fenugreek seeds: Although promising, higher-quality human trials are needed to confirm fenugreek’s effects on glucose control.
Talk with your healthcare provider before adding these foods or supplements if you’re taking diabetes medications, since herbal products can interact with prescriptions.
Also note that the FDA does not regulate supplements like prescription drugs. Choose products tested by independent laboratories for purity and accurate labeling.
Maintain a healthy weight
Keeping a weight appropriate for your height and age supports healthy blood glucose and lowers diabetes risk.
In people with overweight or obesity, even a modest weight loss can improve glucose control and reduce reliance on diabetes drugs.
For instance, someone weighing 200 pounds (91 kg) who loses 10–14 pounds (4.5–6 kg) may notice meaningful improvements in blood glucose.
Losing more than 5% of initial body weight may also improve HbA1c, a marker of average blood glucose over the prior three months.
Opt for healthy snacks more often
Spacing meals and snacks throughout the day can help prevent large swings in blood glucose. Snacking between meals may also lower the risk of type 2 diabetes.
Smaller, more frequent meals can improve insulin sensitivity and reduce blood glucose. This eating pattern may also lower HbA1c, reflecting better average glucose control over three months.
Include probiotic-rich foods
Probiotics — beneficial bacteria — offer many health benefits, including improved blood glucose regulation. In people with type 2 diabetes, probiotics may reduce fasting glucose, HbA1c, and insulin resistance.
A 2016 study reported that glucose improvements were greater when multiple probiotic strains were consumed for at least eight weeks.
Probiotic-rich foods include fermented items such as:
- yogurt labeled with live active cultures
- kefir
- tempeh
- sauerkraut
- kimchi
Frequently asked questions
What are the three signs of hyperglycemia?
Symptoms of hyperglycemia include extreme thirst, frequent urination, blurry vision, fatigue, and wounds that do not heal well.
What are the 3 P’s of diabetes hyperglycemia?
The three P’s are polydipsia (excessive thirst), polyuria (excessive urination), and polyphagia (excessive hunger).
Is type 2 diabetes hypo or hyper?
Type 2 diabetes typically causes hyperglycemia (elevated blood sugar) because insulin’s effectiveness at moving glucose into cells is impaired.
The bottom line
Blood glucose control relies on lifestyle measures such as maintaining a healthy weight, reducing stress, improving sleep, staying active, and staying hydrated. Dietary choices are among the most impactful ways to improve glucose levels.























Leave a Reply
You must be logged in to post a comment.