You’ve heard how everyone’s talking about semaglutide, right? Yeah, you know—the Ozempic headlines, the “miracle weight-loss” hype. But wait a minute, what does that mean if you’ve got type 1 diabetes? Can this drug really help? Or are the risks bigger than the headlines let on? When I first stumbled across a recent clinical trial suggesting semaglutide improved blood sugar and weight loss in adults with type 1 diabetes, I thought, Is this too good to be true? Or worse—is it dangerously misleading? Let’s unpack the facts together. We’ll keep it real, keep it honest, and focus on what matters: your health.
Full disclosure: I’m not selling this drug, and I’m definitely not your doctor. But I’ve read the research, talked to folks managing diabetes, and I’m here to help you get clear, trustworthy answers. Because when it comes to type 1 diabetes treatment, you need the full story—not just the soundbites.
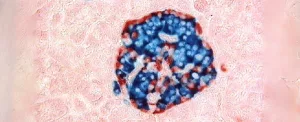
The 2025 Study: What Changed for Type 1 Patients?
Let’s start with the big news you might’ve seen: A diabetes clinical trial in 2025 found that weekly semaglutide helped 36% of adult participants hit a trifecta of improvements—not better blood sugar alone, but weight loss too. No increased risk of ketoacidosis. No more low blood sugar. Just…ah, the relief.
What Exactly Was Tested?
Here’s the setup according to the Oregon Health & Science University (OHSU) study: 72 adults with type 1 diabetes who already used automated insulin delivery systems (like closed-loop pumps) were split into two groups. One got weekly semaglutide injections; the other got a placebo. After 26 weeks, the semaglutide group saw blood sugar stabilization and weight drops averaging 5%. For someone weighing 180lbs? That’s 9 pounds. No crash diet. No doubled-up workouts. Just…medication. Pretty cool, right?
Key Takeaways from the Trial
| Outcome | Semaglutide Group | Placebo Group |
|---|---|---|
| Weight Loss (Avg.) | 5% | 1.2% |
| Blood Sugar Control (A1c) | ↓ 0.3% | No change |
| Insulin Dose Reduction | 17% average decrease | 0% |
Same hypoglycemia risk. Same ketoacidosis incidence. And most importantly… no increased autoimmune panic. But here’s where it gets nuanced: Not everyone responded the same. Some folks dropped weight fast, while others…well, not so much. And that leads us to the next question:
Why Even Consider Semaglutide For Type 1?
So, I get it. Type 1 is different from type 2. Your pancreas doesn’t produce insulin, full stop. But—and this is a big but—your body can still be stressed by “insulin resistance”. Especially if you’re carrying extra weight. Your automatic pump might be smart, but slimming down lightens its load, if you catch my drift.
How Does It Work With Automated Insulin Delivery?
Semaglutide and automated insulin delivery? Seems like a match made in…well, a researcher’s lab. The idea is that semaglutide reduces inflammation, metabolism stress, even appetite. Saves you from binging later. Easier to stay within a target blood glucose range. Like having a teammate whisper, “Hey, cut me some slack—and I’ll help you steady those lows and highs.” That’s how one participant described it in a study write-up: “I still need insulin, but the mental load? Less.”
Side-by-Side: AID + Semaglutide vs. AID Alone
| Metric | AID + Semaglutide | AID Only |
|---|---|---|
| Time in Target Range (BGRs ≈ 70–180 mg/dl) | Increased by 9% of the day | No significant change |
| Insulin Requirements | ↓ 17% | ↑ 3% |
| Psychological Burden of T1D | Self-reported “reduced stress” in 64% of users | Reported as “unchanged” in most |
Certainly, the data sounds exciting. But let’s be honest and real human for a second: This isn’t a cure. It’s not replacing insulin. But maybe—just maybe—it smooths out one corner in an already complicated diabetes picture.
The Weight Loss Puzzle: Unexpected or Too Good?
Here’s another kicker—most folks didn’t sign up for the weight part. They just wanted better semaglutide blood sugar control. But that slimmer number on the scale emerged like a bonus feature. By week 16, people were eating less, cravings dropped, and—surprise—those once-familiar “gym-andZone” attempts weren’t burning them out.
Metallic Appetite Suppression: Is It All In Your Head?
Not really. Behind the scenes, semaglutide mimics GLP-1—a hormone your gut produces that controls hunger and digestion. What automatic insulin delivery does for your glucose, semaglutide does for your cravings and calorie intake. It slows down how fast food leaves your stomach. Makes you hate candy bars before you even unwarp them. As one 11% loss in 6 months patient said, “I wouldn’t say I ‘lost my appetite’… more like I realized three handfuls of chips was never worth that glucose spike anyway.”
What Types of Type 1 Patients Benefit Most?
Pretty much everyone saw modest weight change, but the bigger drops showed up in people already above normal weight. If you’re already thin? Maybe not so much.
Red Flags: The Real Risks You Can’t Skip
Alright, let’s shift gears. Here’s where I have to be the annoying person who says, “But…”
Could Semaglutide Trigger Diabetic Ketoacidosis (DKA)?
We’ve all heard of DKA—and if you live with type 1… you dread it. Now, this isn’t just your typical “day-to-day fluctuation.” We’re talking buildup of ketones. Stomach pain. Extreme thirst. Risky, even unconsciousness. But the 2025 trial only saw one episode in semaglutide users—and zero differences in DKA showing between the groups. That’s promising. Very promising.
But—and I can hear you sighing—this doesn’t rule out a hidden risk. Semaglutide is linked to DKA in some older studies (like those on GLP-1s paired with SGLT2i drugs). And according to Nature, ketoacidosis might still be possible, even without super high blood sugar, known as euglycemic DKA. That’s the kind that sneaks up on you when you least expect it. “Low sugar” might not set off alarms… but your ketones will.
What Precautions Real Patients Should Know
- Check urine ketones if you’re feeling off—even without high BGM.
- Don’t skip insulin checks, especially if your pump needs reprogramming.
- Stock up on urine ketone strips.
- Talk to your endocrinologist before starting any off-label therapy.
What If It Doesn’t Work?
Not everyone saw improved semaglutide weight loss—or clearer blood sugar numbers. In fact, a 2023 study by University at Buffalo found some gained weight again at 12 months. Even with drops in A1c and insulin, some people discovered it’s just… a temporary lift. Also, about 20% dropped out mid-trial due to side effects like nausea and dietary fatigue (again, weight loss fanbase might see that as a gift).
Side Effects You Might Feel
| Mild (common, weeks 1–12) | Severe (rare, but important to notice) |
|---|---|
| Nausea | Dizziness |
| Lightheadedness | Ketoacidosis complaints |
| Reduced Gastro Motility | Gut complications (e.g., ileus—rare though) |
Sounds tough? Yeah, it can. But hey, many diabetes meds aren’t fun. The question is: Are these side effects worth it for what you stand to gain? That’s where we hit the next big issue…
Why Isn’t It Approved Yet?
Hold up—isn’t semaglutide already on the market? Yep. For both type 2 diabetes and obesity, like Wegovy and Ozempic. But with type 1? Still investigational.
The FDA’s Hold-Up: Need Bigger, Longer Data
Look, if I’m the FDA, and only 72 participants tried this over six months, do I rush it through without asking, “What happens after a year? Two?”? Probably not. They’re a stubborn bunch when they need to be.
Understanding Off-Label Prescriptions
So your doctor could prescribe it now. Off-label means the effect might be the same, but no one’s signed off on it specifically. Like using Tupperware for broiles. It works? Maybe. But is it safe for 24/7 meal prep? Jury’s still out.
The 2023 Type 1 Insulin-Use Trials: Hope or Hype?
This isn’t new territory. A 2023 University at Buffalo study lit up the blog posts. They gave semaglutide to recently diagnosed T1D patients with automatic glory. Results? Crazy: Two-thirds halved their insulin use within months. Some slid sideways:
One Patient’s Story
“It’s weird. My appetite shifted. I genuinely didn’t want pizza or ice cream anymore. Combine that with less insulin guesstimates each day… Yeah, my stress tanked according to my blood log. But if I’d done this alone? Probably overdosed.”
Bright side? Less insulin needed. Downside? Any drastic shift could backfire—especially if you’ve got a history of DKA. That’s why pairing this with a medical team is non-negotiable.
But Wait…Longer-Term Outcomes?
If we zoom further back, the same researchers did a 12-month follow-up. Bad news: some people hit a plateau. Or—worse—reversed back. That’s the problem when we’re relying on 6-month data. We need to see deeper into the forest. Maybe 18 or 24 months.
The Big “Medical vs. Benefit” Puzzle
Right now, semaglutide isn’t a slam dunk. If it were, the stand-up version would be dumped in every community pharmacy. The issue isn’t the drug itself. It’s whether your body reacts the right way.
Is Everyone Eligible, or Only In Specific Circumstances?
Legit question. Let’s get this in numbers: in most trials, patients were overweight. BMI hovered above 28 in that OHSU study. So, if your metabolism reads arrhythmic, and your insulin requirements feel real messy, maybe this is worth a chat. But if you’re already very lean? Semaglutide might not offer as much.
Back in 2024: How Did Early-Stage Type 1 Patients React?
Here’s where the honeymoon phase gets complicated—with its help, folks in early type 1 lasted longer on less insulin when coupled with mild dietary changes a 2024 trial from NEJM showed. That gives you more adaptability, and your mind feels less pressure when your belly isn’t ravenous. But again, this isn’t a guarantee. Diabetes is flexible—but your risk curves depend on your gut, your metabolism, your habits.
So… Should You Try Semaglutide?
Here’s the moment where we both take a deep breath. Semaglutide isn’t replacing insulin care for type 1. But if it helps lower the number of pricking yourself, reduce pump adjustments, and take the weight off without being miserable—then maybe it’s worth giving careful consideration.
Balance Over Hype
This is what’s so frustrating. Investment-grade messaging wants to scream, “Miracle!” and accuracy must whisper, “With caution.” The authors of the 2025 OHSU trial said it themselves: You still need insulin. If you ignore that—even dial down coverage—you risk DKA in a wicked hurry.
And the weight loss isn’t permanent. One 2024 report from Nature noted that people stopped losing after hitting a certain point. “The drug doesn’t attack belly fat or squeeze muscle tone onto legs. It just shifts how you intake calories—and even then, consistency matters.”
What Should You Ask Your Diabetes Doctor?
Okay, you’re sold on giving it a try. But before hitting “chat with insurance,” definitely ask your type 1 care team:
- Am I in the nearly overweight range for a reason this might help?
- Will I need ketone monitoring at home for safety?
- Is my pump integrating current data with new semaglutide use, or is recalibration needed?
- What’s our Plan B if I’m struggling with side effects, or worse, rebound weight gain?
Bottom Line: An Urgent Step Forward, Not a Leap
If you’re living with type 1 diabetes treatment, this might feel like a long-awaited possibility. And I get it—after years juggling carb counting, timing, and pump rage days, you dream of anything that helps.
What this 2025 clinical trial actually showed isn’t that semaglutide is a “magic bullet.” You still need insulin. You still have to test often. You still have diabetes.
What it does do: Gives you a possible chance to cut insulin need. Maybe soften spikes. and finally, maybe the half of the diabetes management scales that’s emotional—from fatigue, from feeling trapped… well, maybe that feels lighter. Like a friend took over a small task for you.
But don’t rush. I’m not a doctor, and neither is the “guy next to you on Reddit who tried it.” Talk slowly, and double back. Ask: “What happens if I stop it? Repeat DKA?”
What I can do: help you get this data into language you can use when talking to your provider or insulin pump rep. There are intakes where you see weight loss despite your diabetes fights—and that’s peace of mind.
Because when you’ve got type 1 injuries on your plate… sometimes, anything that makes it less of a rollercoaster? It’s… welcome. Even if it’s not a coronary bypass.
What do you think? Ready to ask your endocrinologist about the semaglutide weight loss angle—or do you prefer to wait? Leave your experience in the comments below (not going to study it with a blood-glucose Excel, but we’re all ears).
























Leave a Reply
You must be logged in to post a comment.