So, here’s the thing
Let’s not sugarcoat this. The same diet that fuels your late-night cravings — the fast food, the sugar bombs, the sedentize (you know, that mix of sitting too long and eating too much) — is getting a serious side-eye for why young adults are increasingly getting diagnosed with gastrointestinal cancers.
Yeah, real talk: we’re seeing more and more 20-somethings and 30-somethings showing up to colonoscopies with results that should’ve taken decades longer to materialize. And it’s not just colorectal cancer. Stomach, pancreatic, even esophageal cases are on the rise, and doctors are scrambling to figure out why. But one major suspect keeps popping up: our habits from adolescence are ghosting us in adulthood.
What’s driving the GI cancer trend in the young?”
When a 43-year-old dies from colorectal cancer — like Chadwick Boseman did — people pay attention. He wasn’t a smoker, he wasn’t “high risk” in the traditional sense. He was just… a guy who probably had a diet that looked more processed than Hollywood green screen. And he’s not alone. Data shows a 14.8% jump in GI cancer cases among young adults between 2010 and 2019 alone.
But this isn’t some random spike — it’s a pattern. A JAMA review analyzed over 115 studies and found that while we’ve gotten better at treating older patients, the younger group — ages 20 to 49 — is falling behind in both early detection and lifestyle habits.
The kicker? The spike isn’t evenly spread. Hispanic and Asian young adults have nearly 3.5x the risk, and those in lower-income neighborhoods are more likely to show up at doctors’ offices with Stage IV diagnoses. Why? Because they either didn’t know the signs or couldn’t access timely care.
How your teen snack habits might come back to bite you now
“What the hell does eating hot pockets at 17 have to do with a gut cancer diagnosis at 30?” Great question. You’ll want to hear this bit: scientists at the University of California found a powerful gut toxin — produced by E. coli bacteria — has a direct link with early-onset colorectal cancer. And guess what diet turbocharges this little menace? Yep, the one loaded with ultra-processed, sugar-heavy, fast-food options.
This stuff isn’t just theory. A study in Nature tracked close to 1,000 patients diagnosed before age 55. The majority of them had genetic mutations that pointed to bacterial damage — not just from last week’s sushi roll, but from toxins that took root way earlier, sometimes before puberty.
“It’s like a ticking time bomb, set off by teenage pizza,” says Dr. Alexandrov, the lead researcher. “If your gut environment was messed up 20 years ago, then you’re seeing the fallout today, even if you improved your habits later.”
Genes vs. habits — which one actually slaps you with cancer?
You might think, “Well, maybe my family got it. So I’m just outta luck.” But listen: Only 15-30% of GI cancers in young adults are actually hereditary. The rest? Driven by daily life. That includes:
- Heavy soda consumption
- Low fiber intake
- Constant antibiotic overuse
- And yes, even microplastics
Let me say that again. Most early-onset cancers aren’t just genetic — they’re lifestyle-driven. So if you’re wondering why your friend who never eats a vegetable got bad news from a doctor and you’re still fine, this is why: it’s not all luck, it’s what you’ve been feeding your guts (literally) since you were old enough to choose what you eat.
Here’s the other part you probably didn’t consider: obesity has been linked to nearly 85% of early-onset GI cases. That’s not “every single one.” But the trend is undeniable — weight gain and poor digestion over the last 20 years have left a mark, even before folks realize it.
What are the odds of getting a GI cancer diagnosis before 50?
If you were born in 1990 or later, you’ve got twice the colon cancer risk and four times the rectal cancer risk compared to someone born in 1950 — even if you’re eating healthy now. The damage is cumulative. And if you were into sodas or processed foods back in your teens or 20s, you might be seeing the impact in your 30s or 40s.
Still think it’s not relevant? Here’s a stat to shock you: In 2022, the US diagnosed 21,001 young adults with GI cancer. That’s 21,001 people who thought — like you might — that they were “too young for cancer.” That number doesn’t include early-onset stomach or pancreatic cancer, both of which are ticking upward, even as older age groups see a general decline in cancer rates.
GI cancer symptoms aren’t subtle, but you keep shrugging them off
“What does a gastrointestinal cancer feel like anyway?” I’m glad you asked. Most aren’t dramatic like chest pain. But they are persistent — and often get brushed aside as “just digestion.” Let’s walk through the signs people actually miss:
- Bloatedness that doesn’t go away
- Changes in your stool — loose, narrow, or bloody
- Unexpected weight loss (even if you thought you were just burning muscle)
- Stomach pain that won’t quit
Here’s the problem: a lot of folks just slap on more Tums or chalk it up to “too much soda” and move on. But if it doesn’t get better in a few weeks, then you better not wait another five. Especially if your family history has a cancer chapter of their own.
And if you’re feeling off, even if you’re active, lean, and eat better now — don’t just hope it’s stress. Because some tumors grow aggressively and quietly in younger people, often without the typical warning of polyps. It’s not “just getting old” when you’re still in your 30s.
Screening age just got lower — and yes, you should care
Doctors used to wait until 50 to start pushing colonoscopies. That’s changed. The American Cancer Society says you should start screenings at 45 years old, even if you’re at average risk. And for those with a family history of Lynch syndrome, early-onset colorectal cancer, or CDH1 issues? Your doc might suggest you test sooner. Like, in your early 30s or even 20s.
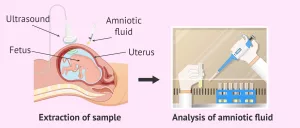
The options are simple: a stool test (at home, cheap, and painless) or a full colonoscopy (the real deal but with a full prep — you’ve heard the horror stories). The good news? The stool test now flags cancer mutations early, and if anything seems off, your doctor will push for the follow-up.
Not seeing your doctor anytime soon? Don’t wait. If you’ve had persistent gut discomfort for a few weeks now, especially if you’re under 50, bring it up at your next appointment. Because catching this early changes survival stats — 94% at early stages, versus 21% at stage IV — and you might be one of the ones who catches it early, if you just care enough to ask.
Can you prevent GI cancer even if you’re not genetically at high risk?
Absolutely, yes. Here’s the catch: You have to treat your gut like it’s still worth investing in. Because if you thought your 20s gave you a free pass, that fantasy is now a health hazard. And the data is clear. If you’re looking to stay ahead of the GI cancer curve (and avoid waking up with bad news at 38), here’s what to tackle now:
- Swap out sugary drinks — even diet soda. One study showed that regular soda drinkers in their teens are 85% more likely to get early-stage colorectal cancer by 40.
- Move more than the couch — like I said, sitting is part of the disease. If you’ve been a Zoomie, a desk-dweller, or just straight up sedentary, your gut is not happy. And yeah, it shows on scans.
- Build a real grocery list — ditch processed foods if possible. Eat more fiber, leafy greens, and even fermented ones like kimchi or sauerkraut (gross, but powerful for gut flora).
If your response is “I eat healthy,” cool — but don’t just stop there. Gut bacteria take years to shift. And if your microbiome has been trashed by antibiotics or microplastics (yeah, those get into the gut too), your best move is not just to eat clean now, but to get a stool DNA test before 45. Because waiting until you’re “old enough” for screenings might be waiting too long.
Here’s the gut check — pun intended
If you’re under 50 and reading this, you’re not out of the woods. Gastrointestinal cancers are growing faster in your age group than in older adults, and while that sounds heavy, it doesn’t mean you’re helpless. The best part? Small moves add up. Drinking less, moving more, and talking to your doctor before you hit 40 about a stool-based screening — even if you’re not symptomatic yet.
Don’t be like Dr. Ryan O’Grady, who shrugged off symptoms until after a vacation to Disney World — and ended up with a diagnosis right before Christmas. Yeah, real talk, that’s not a story you want to share in casual conversation. He was 43, a math professor, not some “high-risk” poster patient. But his habits? Soda, late-night pizza, minimal exercise — told the opposite story. That’s the truth.
You’ve got a shot. Start now. Make a move that matters. And if you know someone who fits this trend — share this with them. Because the goal isn’t just to avoid GI cancer symptoms in your 30s and 40s. It’s to not be part of that 14.8% rise in early-onset cancers over the last decade. You’ve got control. Use it.





















Leave a Reply
You must be logged in to post a comment.