Hey there, friend. If you’ve just stopped a steroid cream and suddenly feel like your skin’s on fire, you’re probably not dreaming—you’re likely dealing with topical steroid withdrawal. It’s a real, sometimes scary, rebound that can turn a helpful medication into a painful mystery.
Below you’ll find the quick‑read you need: what the condition looks like, why it happens, how to taper safely, and which soothing treatments actually work. Grab a cup of tea, settle in, and let’s untangle this together.
What is TSW
Topical Steroid Withdrawal (TSW), also called Topical Steroid Addiction or Red Burning Skin Syndrome, is a rebound inflammation that appears after you stop using moderate‑to‑high potency topical corticosteroids for a while. The skin’s natural barrier has become dependent on the steroid’s anti‑inflammatory power, so when the drug disappears, the body over‑reacts.
The condition is recognized by dermatologists worldwide and listed under ICD‑10 codes F55.3 and L71.0. For a solid clinical overview, see DermNet.
Think of it like walking away from a favorite coffee after weeks of daily cups—the body craves that hit of caffeine and reacts when it’s gone. Except, in this case, the “caffeine” is a steroid, and the withdrawal can make your skin feel like a furnace.
Common Symptoms
| Symptom | Typical Onset | What It Feels Like |
|---|---|---|
| Red, burning skin | Hours‑days | Flushed, hot, often on the face, neck, or periorificial areas |
| Intense itching | 1‑3 days | “Pins and needles” that can keep you up at night |
| Scaling / peeling | 3‑7 days | Dry, flaky patches that may look like sunburn |
| Swelling / papules | Variable | Small bumps or puffiness, sometimes mistaken for rosacea |
| Systemic signs (headache, nausea) | Rare | General “blah” feeling; often reported in long‑term cases |
Many people think they’re just having a flare‑up of eczema, but the pattern is different. The redness often spreads in a “face‑and‑nose” distribution, and the burning sensation is far more intense than usual eczema itch.
A powerful illustration comes from Alicia’s five‑month journey, shared on ITSAN. She described waking up with a “bright, fire‑red face” that never cooled, despite using stronger creams. Real‑world stories like hers turn abstract symptoms into something we can truly empathize with.
Side Effects
While you’re on topical steroids, the drugs have their own set of side effects. Knowing them helps you weigh the risk‑reward balance before deciding to stop or continue.
- Skin thinning & striae: Prolonged use of potent steroids can make the skin fragile, leading to stretch marks.
- Telangiectasia (spider veins): Tiny blood vessels become visible, especially on the face.
- Steroid‑induced rosacea: Red bumps that mimic acne.
- Systemic absorption: In rare cases, especially with high potency over large areas, the drug can suppress the hypothalamic‑pituitary‑adrenal (HPA) axis.
The UK government’s Medicines and Healthcare products Regulatory Agency (MHRA) outlines these risks in its safety leaflet topical corticosteroids and withdrawal reactions. The key takeaway? Stick to the prescribed strength and duration—usually no more than two weeks of continuous use for medium‑to‑high potency steroids.
Taper Safely
Stopping cold turkey is the fastest route to a full‑blown withdrawal flare. Instead, a gentle taper lets your skin adjust gradually. Below is a practical, friend‑to‑friend taper plan you can discuss with your dermatologist.
General Principles
- Step down the potency: Move from super‑potent (e.g., clobetasol) to milder options (e.g., hydrocortisone 1%).
- Reduce application frequency: Daily → every other day → twice a week.
- Keep a “test spot”: Apply the new regimen to a small area of forearm first; watch for rebound before expanding.
- Support the barrier: Use plain emollients (petrolatum or ceramide‑rich creams) liberally.
Sample 6‑Week Taper
| Week | Strength | Frequency |
|---|---|---|
| 1‑2 | Super‑potent (clobetasol) | Once daily on worst spots |
| 3‑4 | Mid‑potent (betamethasone) | Every other day |
| 5‑6 | Low‑potent (hydrocortisone 1%) | Twice weekly |
| 7+ | None (just moisturiser) | As needed |
Every person’s skin is unique, so feel free to stretch or compress weeks based on how you feel. If the burning spikes, pause a week at that level and add a soothing barrier cream.
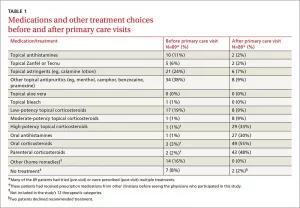
Treatment Options
Once withdrawal symptoms appear, you’ll want more than just “wait it out.” Below are evidence‑based, friend‑recommended treatments that actually bring relief.
Supportive Skin Care
- Plain moisturisers: Look for products with petrolatum, dimethicone, or ceramides. They lock in moisture and repair the lipid barrier.
- Wet‑wraps: Dampen a clean cloth, wrap it around the affected area, then cover with a dry layer. This reduces itch and speeds healing.
- Cool compresses: A cool (not icy) washcloth for 10‑15 minutes can calm that burning sensation.
Pharmacologic Aids
- Oral antihistamines: Cetirizine or diphenhydramine can curb nocturnal itching.
- Low‑dose oral steroids: Only under strict medical supervision, and usually for a brief “bridge” period to control severe rebound.
- Doxycycline: Helpful when the rash resembles rosacea because it has anti‑inflammatory properties.
Alternative & Adjunct Therapies
- Oatmeal baths – soothing and anti‑itch.
- Calamine lotion – cool, drying effect for pustular patches.
- Probiotic‑rich skin care – emerging research suggests gut‑skin axis support may aid recovery (still early, but promising).
Julia, another ITSAN member, found that a ceramide‑rich ointment paired with regular wet‑wraps cut her itching in half within a week. She credits the combination of “smart skincare + a good taper plan” for getting her back on her feet.
Prevention Tips
Wouldn’t it be great if you could avoid withdrawal altogether? Here are habit‑forming practices that keep steroids a short‑term helper rather than a long‑term crutch.
- Follow the prescribed duration: Most dermatologists recommend no more than two weeks of continuous use for potent steroids.
- Rotate with non‑steroidal options: Calcineurin inhibitors (tacrolimus, pimecrolimus) work well for chronic eczema without the rebound risk.
- Maintain a Steroid Use Log: Jot down the brand, strength, start date, and stop date. Seeing the timeline on paper makes it easier to stick to limits.
- Schedule regular skin check‑ups: Every 3‑6 months for chronic conditions ensures early detection of any over‑use patterns.
And, of course, always discuss any plan to stop or taper with a qualified clinician. A quick phone call can save months of frustration.
Resources
Want to dive deeper? The following trusted sources let you explore the science, find community support, and download handy tools:
- DermNet – detailed clinical guide
- ITSAN – global TSW community and personal stories
- UK MHRA – safety leaflet on topical steroids
- Downloadable taper chart (PDF) – keep it on your phone for quick reference.
Conclusion
Topical steroid withdrawal is a real, often‑misunderstood rebound that can turn a helpful cream into a painful nightmare. By recognizing the warning signs, tapering gradually, and leaning on supportive skin care, most people can weather the storm without permanent damage. Your skin will thank you for the gentle, informed approach.
Remember: track every steroid you use, talk openly with your dermatologist before making changes, and don’t hesitate to reach out to supportive communities like ITSAN. If you have questions, personal tips, or just need a listening ear, drop a comment below. We’re all in this together, and together we’ll get your skin back to feeling calm and comfortable.





















Leave a Reply
You must be logged in to post a comment.