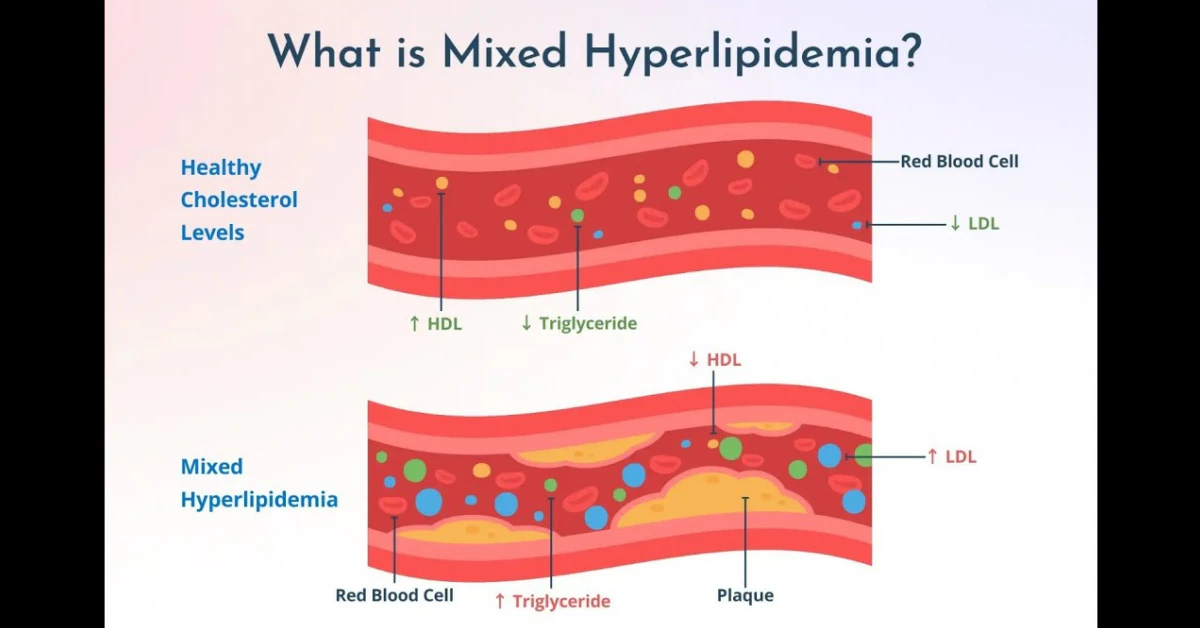
Mixed hyperlipidemia is a condition that raises both “bad” cholesterol (LDL) and triglycerides at the same time, putting your heart at higher risk. In plain English: the blood‑fat picture is “mixed,” so you’re dealing with more than one type of lipid that can clog arteries.
Stick around and I’ll walk you through what it really means, why it shows up, how doctors spot it, the best ways to treat it, and what it could mean for your life expectancy. Think of this as a friendly chat over coffee—no jargon, just clear answers you can use today.
Definition & Meaning
What is mixed hyperlipidemia?
Mixed hyperlipidemia, also called familial combined hyperlipidemia or mixed dyslipidemia, is an inherited disorder where the body produces high levels of low‑density lipoprotein (LDL) cholesterol and triglycerides, often with lower high‑density lipoprotein (HDL). It’s one of the most common inherited lipid problems, affecting roughly 1 in 100 people — according to Healthgrades.
Mixed hyperlipidemia vs. other lipid disorders
If you’ve heard of “high cholesterol,” that usually refers to isolated LDL elevation. Mixed hyperlipidemia, on the other hand, is a “combo‑meal” for your arteries: LDL plus triglycerides (and sometimes low HDL). The combination makes the cardiovascular risk jump higher than any single abnormality alone.
ICD‑10 code
In the medical record, mixed hyperlipidemia is coded as E78.2. If you ever need to look up the code for insurance or a specialist visit, that’s the one to ask for.
| Lab Parameter | Typical Range (mg/dL) | Mixed Hyperlipidemia Threshold |
|---|---|---|
| Total Cholesterol | <200 | >200 |
| LDL‑C | <100 (optimal) | >130 |
| Triglycerides | <150 | >170 (fasting) |
| HDL‑C | 40‑60 (men), 50‑60 (women) | <40 (men) / <50 (women) |
Causes & Risks
Genetic inheritance
The “familial” part isn’t just a buzzword. Studies show an autosomal‑dominant pattern: if one parent carries the gene, there’s about a 50 % chance you’ll inherit it. Some families even have a “double‑dose” when both parents are affected, leading to higher lipid levels earlier in life.
Lifestyle and metabolic contributors
Genes set the stage, but what you eat, how you move, and other habits can dramatically amplify the problem. A sedentary lifestyle, a diet rich in saturated fats and simple sugars, excess alcohol, or chronic obesity can push triglycerides sky‑high and worsen LDL. In fact, mixed hyperlipidemia often shows up alongside metabolic syndrome—a cluster of high blood pressure, high blood sugar, and abdominal obesity—as highlighted by a BMJ review (BMJ 2011).
Medical conditions that aggravate it
- Type 2 diabetes
- Hypothyroidism
- Polycystic ovary syndrome (PCOS)
- Non‑alcoholic fatty liver disease (NAFLD)
- Chronic kidney disease
Emerging research
Scientists are still hunting for the exact gene culprits—APOA5, LDLR, and a handful of others are in the spotlight. While the science evolves, the practical advice stays the same: know your family history and keep an eye on your numbers.
Symptoms & Signs
What symptoms might you notice?
The tricky part is that many people feel perfectly fine. Mixed hyperlipidemia is often discovered on a routine blood test. When symptoms do appear, they’re usually skin or cardiovascular clues:
- Xanthomas: yellowish, fatty deposits on elbows, knees, or eyelids.
- Arcus corneae: a white‑gray ring around the cornea of the eye.
- Chest pain or angina: due to narrowed coronary arteries.
- Leg cramping during exercise: a sign of peripheral artery disease.
- Early heart attacks or strokes: especially if there’s a strong family history.
When to get worried
If you suddenly develop chest pain, unexplained leg pain, or notice xanthomas, call your doctor right away. These “red‑flag” signs mean the excess lipids may already be damaging vessels.
Diagnosis & Tests
Which blood tests confirm it?
The cornerstone is a fasting lipid panel. You’ll need four numbers:
- Total cholesterol
- LDL‑C
- HDL‑C
- Triglycerides (fasting)
Mixed hyperlipidemia is generally diagnosed when fasting triglycerides exceed 170 mg/dL and total cholesterol is above 200 mg/dL, per the BMJ criteria mentioned earlier.
What if LDL can’t be calculated?
When triglycerides soar above 400 mg/dL, the traditional Friedewald equation fails. In those cases, labs either run a direct LDL assay or use newer formulas (e.g., Martin/Hopkins). Ask your provider which method they’re using.
Is genetic testing necessary?
Only if the family history is strong, the diagnosis is unclear, or you’re planning to involve a specialist in lipid genetics. Testing can be pricey, so weigh the benefit—knowing the exact mutation might guide therapeutic choices, especially for rare variants.
Treatment Options
What is mixed hyperlipidemia treatment?
Goal‑setting is simple: lower LDL under 100 mg/dL, bring triglycerides under 150 mg/dL, and raise HDL a bit if possible. Reaching those targets slashes your heart‑attack risk dramatically.
Lifestyle first
Think of lifestyle changes as the foundation—like laying a solid floor before adding furniture (medications). Here’s a quick “starter kit”:
- Heart‑healthy diet: Mediterranean‑style meals—plenty of fish, olive oil, nuts, fresh veggies, and whole grains. Cut saturated fats, trans fats, and sugary drinks.
- Exercise: Aim for at least 150 minutes of moderate‑intensity activity each week—think brisk walks, cycling, or dancing.
- Weight management: Losing 5‑10 % of body weight can drop triglycerides by up to 20 %.
- Alcohol moderation: Keep intake below two drinks a day for men and one for women.
- Quit smoking: Smoking spikes LDL and lowers HDL—quitting is a double win.
Medication toolbox
If lifestyle alone isn’t enough (and it often isn’t), medications step in.
- Statins (first‑line): Atorvastatin, rosuvastatin, and others lower LDL by 30‑50 % and modestly reduce triglycerides. Typical doses range from 10 mg to 80 mg.
- Fibrates: Fenofibrate or gemfibrozil target high triglycerides and modestly raise HDL. Useful when TG > 300 mg/dL.
- Ezetimibe: Blocks cholesterol absorption; often added to a statin if LDL isn’t at target.
- PCSK9 inhibitors: Alirocumab or evolocumab—injectable, powerful LDL‑lowering agents for resistant cases.
- Combination therapy: A statin plus a fibrate is common for mixed presentations—a strategy supported by the DrOracle AI article that notes the synergy of statins and fenofibrate.
Monitoring & follow‑up
After you start or adjust therapy, repeat the lipid panel in 4‑12 weeks. Once stable, check annually—or more often if you have diabetes, kidney disease, or a strong family history.
Special situations
- Pregnancy: Statins are contraindicated. Focus on diet, omega‑3 fatty acids, and safe exercise.
- Diabetes: Tight glucose control helps lower triglycerides; some diabetes meds (e.g., GLP‑1 agonists) also improve lipid profiles.
- Kidney disease: Dose‑adjust certain statins; avoid high‑dose fibrates if eGFR < 30 mL/min.
Prognosis & Life
How does it affect life expectancy?
Untreated mixed hyperlipidemia can trim years off your life because of premature cardiovascular disease. A study from Medicover Hospitals (Medicover) notes a clear link between the disorder and reduced life expectancy, mainly from heart attacks and strokes.
Good news: aggressive treatment—statins, lifestyle changes, and regular monitoring—can bring your risk back down to that of the general population. In other words, the condition doesn’t have to be a death sentence.
Risk reduction numbers
Large randomized trials show statins cut major cardiovascular events by roughly 30 % and overall mortality by about 10‑15 % in high‑risk groups. Adding a fibrate when triglycerides stay high can shave another few percentage points off the risk of heart attacks.
Long‑term outlook
When you keep LDL under 100 mg/dL and TG under 150 mg/dL, most people live a normal lifespan and enjoy the same quality of life as someone without the disorder. Consistency is key—think of your heart as a garden that needs regular watering and weeding.
Practical Steps
Self‑check checklist
- Do you have a family member with early heart disease?
- Has a doctor ever mentioned “high cholesterol” or “high triglycerides”?
- Do you have any of the following: obesity, high blood pressure, diabetes, or a sedentary lifestyle?
- Have you had a fasting lipid panel in the past year?
Preparing for your appointment
Bring a list of any medications (including over‑the‑counter supplements), a fasted blood‑test report if you have one, and notes about your diet and exercise habits. Ask these questions:
- What are my exact LDL, HDL, and triglyceride numbers?
- Do I need a genetic work‑up?
- Which medication(s) do you recommend and why?
- How often should we repeat labs?
Sample questions for your doctor
“If I start a statin, what side effects should I watch for?”
“Would a combination of statin and fibrate be better for my numbers?”
“Can I get a diet plan that fits my cultural preferences?”
Trusted Resources
For deeper dives, consider these reputable sources (always discuss what you read with your clinician):
- HealthGrades – Mixed Hyperlipidemia: Causes, Symptoms, and Treatment
- BMJ – Investigating mixed hyperlipidaemia (2011)
- National Lipid Association guidelines (latest recommendations)
- American Heart Association – Education on cholesterol management
Conclusion
Mixed hyperlipidemia may sound intimidating, but it’s a manageable condition when you know the facts and act early. By understanding that it’s a “mixed” lipid problem, getting regular blood tests, embracing a heart‑healthy lifestyle, and following evidence‑based medication plans, you can dramatically lower your cardiovascular risk and preserve a full, vibrant life.
So, what’s your next step? Schedule a fasting lipid panel, talk to a trusted healthcare provider, and start a small, sustainable change today—whether it’s swapping a sugary snack for a piece of fruit or adding a brisk 20‑minute walk to your routine. Your heart will thank you, and you’ll feel more empowered every day.






















Leave a Reply
You must be logged in to post a comment.