Hey there! If you’ve ever woken up with a stiff, throbbing joint that just won’t quit, you’re not alone. Inflammatory joint diseases can feel like an uninvited guest that shows up without warning, brings the whole house down, and stays for far too long. The good news? Knowing what’s happening under the surface, why it happens, and how you can take charge makes a massive difference. Let’s sit down (preferably on a comfy chair), have a friendly chat, and untangle the mystery together.
What Are They?
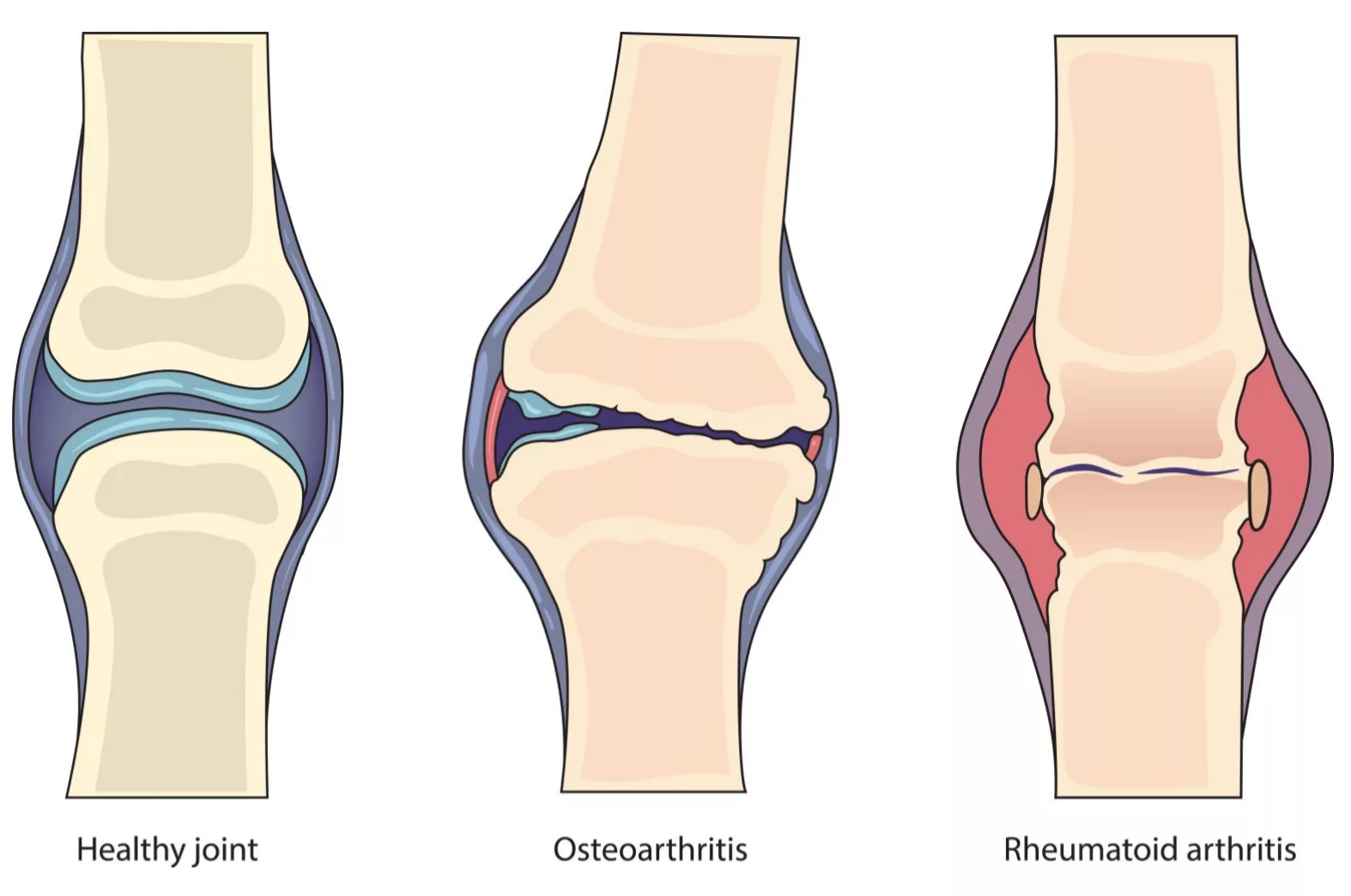
Inflammatory joint diseases are a family of conditions where the immune system decides to “attack” the lining of your joints instead of protecting them. Think of it as a traffic jam inside the joint: immune cells flood the area, release inflammatory chemicals, and cause swelling, pain, and sometimes permanent damage. It’s different from the good‑old wear‑and‑tear we call osteoarthritis; here the body’s own defenses go rogue.
Key Types
There are several familiar faces in this crowd:
- Rheumatoid arthritis (RA) – often starts in the small joints of the hands and feet and spreads.
- Gout and calcium pyrophosphate deposition disease (CPPD) – crystal‑driven inflammation that can flare up suddenly. Want the low‑down on these crystals? Check out gout and CPPD.
- Spondyloarthropathies – includes ankylosing spondylitis and psoriatic arthritis, which love the spine and entheses (the spots where tendons attach).
- Other rarer forms – like lupus arthritis, juvenile idiopathic arthritis, and septic arthritis.
All of them share the same core problem: inflammation that, if left unchecked, can damage cartilage, bone, and the delicate synovial membrane that lubricates the joint.
Why It Matters
Why should you care about a label? Because these diseases affect millions worldwide and can steal precious moments of mobility, independence, and joy. Early detection can stop the train before it derails your daily routine. Plus, the treatments available today are far better than they were a decade ago – we’ve gone from “just rest” to targeted medicines that keep the immune system in check.
How It Starts
Understanding the root helps you understand the remedy. Here’s a quick tour of the inner workings:
- Immune‑cell infiltration – T‑cells, B‑cells, and especially macrophages march into the joint lining, releasing cytokines like TNF‑α, IL‑1β, and IL‑6. These chemicals amplify the fire.
- Macrophage pathways – When macrophages encounter danger signals, they trigger the NLRP3 inflammasome, which releases even more IL‑1β. This is a key driver in both RA and crystal‑driven inflammation.
- Crystal‑driven inflammation – Tiny shards of uric acid (gout) or calcium pyrophosphate (CPPD) act like splinters, provoking the immune system. For a deeper dive, see crystal-driven inflammation.
According to a study published in Nature Reviews Rheumatology, targeting these cytokines early can halt joint erosion in up to 70% of patients (source).
Risk Factors
Not everyone with a genetic predisposition will develop disease, but certain triggers tip the scales:
- Genetics – specific HLA‑DRB1 alleles increase RA risk.
- Toxic particle exposure – inhaling silica, asbestos, or other fine particles primes macrophages in the lungs, leading to systemic inflammation that can aggravate joint disease. Learn more about these connections in toxic particle diseases.
- Silicosis causes – chronic silica inhalation not only damages lungs but also fuels the inflammatory cascade that can affect joints (silicosis causes).
- Lifestyle – smoking, obesity, and a diet rich in purines (think red meat and seafood) raise the odds of gout and can worsen RA.
- Co‑morbidities – kidney disease, metabolic syndrome, and even chronic infections can act as hidden saboteurs.
Getting Diagnosed
Diagnosing inflammatory joint diseases is a bit like detective work. Here’s what doctors usually do:
- History & physical – They’ll ask about morning stiffness (lasting >30 minutes is a red flag), swelling patterns, and family history.
- Lab tests – Rheumatoid factor (RF), anti‑CCP antibodies (highly specific for RA), ESR/CRP (general inflammation markers), and uric acid levels for gout.
- Imaging – X‑rays reveal erosions, ultrasound can spot crystal deposits, and MRI shows early bone marrow edema.
- Joint aspiration – Pulling fluid from a swollen joint can confirm crystals or rule out infection (septic arthritis).
When a physician suspects infection, they’ll order a culture, because septic arthritis demands immediate antibiotics and sometimes surgery.
Treatment Options
Now for the hopeful part – there are many ways to tame the fire.
Pharmacologic Backbone
- NSAIDs – ibuprofen or naproxen for quick pain relief.
- Conventional DMARDs – methotrexate, sulfasalazine, and leflunomide slow disease progression.
- Biologic agents – TNF inhibitors (adalimumab, etanercept), IL‑6 blockers (tocilizumab), and newer JAK inhibitors (tofacitinib). These target the exact cytokines we talked about.
- Crystal‑specific meds – colchicine for acute gout flares, and urate‑lowering drugs like allopurinol or febuxostat for long‑term control.
Non‑Pharmacologic Adjuncts
- Physical therapy – gentle range‑of‑motion exercises keep joints supple.
- Occupational therapy – tools like ergonomic kitchen gadgets reduce strain.
- Diet tweaks – a Mediterranean‑style diet, low in purines and refined sugars, can lower inflammation.
- Weight management – every 5 kg lost reduces joint load dramatically.
Emerging & Niche Therapies
Science never sleeps. Recent trials show promise for IL‑17 blockers in axial spondyloarthritis, and some clinics are experimenting with regenerative options (PRP, stem‑cell injections) for patients who still have pain despite optimal medical therapy. As a rheumatologist once told me, “Regeneration is a beautiful supplement, but you still need the immune system in check first.”
Monitoring & Follow‑Up
Regular labs (every 3‑6 months) and imaging when symptoms change keep the treatment plan on track. Patient‑reported outcome measures—simple questionnaires about pain and function—help doctors see the bigger picture.
Living Well
Managing a chronic condition is a marathon, not a sprint. Here are some everyday habits that make the journey smoother:
- Stay active – low‑impact activities like swimming, cycling, or yoga keep joints moving without pounding them.
- Quit smoking – it not only reduces flare‑ups but also improves the effectiveness of biologic drugs.
- Mind your mental health – chronic pain can be draining. Mindfulness, CBT, or a supportive friend group can be game‑changers.
- Footwear matters – well‑fitted shoes with good arch support ease pressure on the knees and hips.
- Regular check‑ins – schedule rheumatology appointments even when you feel good; prevention beats reaction.
Remember, you’re not fighting this alone. Support groups, online forums, and knowledgeable clinicians are all part of your toolbox.
Expert Insights
To give you a taste of real‑world experience, here are two quick case snippets:
- Mark, 45, construction worker – Years of silica dust exposure led to early‑onset RA despite a non‑smoker status. After a rheumatology referral, he started a TNF inhibitor and now enjoys weekend hikes again.
- Lena, 58, avid home‑cook – Recurrent gout attacks after a fondness for steak and beer. A simple switch to a low‑purine diet, coupled with allopurinol, reduced flares from monthly to yearly.
Both stories illustrate the power of combining lifestyle tweaks with targeted medication.
Takeaway & Next Steps
Inflammatory joint diseases can feel overwhelming, but knowledge is your greatest ally. By recognizing the signs early, understanding the underlying immune pathways, and embracing a balanced treatment plan, you can reclaim mobility and enjoy life’s little pleasures—whether that’s dancing at a wedding, gardening, or simply walking the dog without wincing.
If any of this resonated with you, consider scheduling a chat with your primary care provider or a rheumatologist. Bring a list of your symptoms, any family history, and be honest about lifestyle factors. The sooner you act, the better your chances of keeping those joints happy and healthy.
What’s your story? Have you found a particular habit or treatment that’s helped you feel more in control? Feel free to share—every experience adds to the collective wisdom we all need.




















Leave a Reply
You must be logged in to post a comment.