Hey there, mama‑to‑be! If you’ve ever curled up with a tissue box because sneezing feels like an avalanche, you know how frustrating allergies can be—especially when you’re expecting. The good news? Most antihistamines on the shelves today are pretty friendly to a growing baby. The not‑so‑good news? A few of them can raise eyebrows, especially in the first trimester. Let’s walk through what’s safe, what to avoid, and how to make the right call for you and your little one.
What Are Antihistamines?
Antihistamines are meds that block histamine, the chemical your body releases when you sniff pollen, pet dander, or even a cold. By shutting off histamine’s “run‑away” signals, they calm itching, sneezing, runny noses, and that annoying watery‑eye feeling. They come in two families:
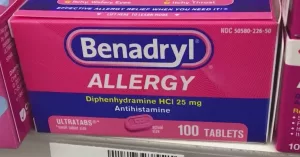
- First‑generation (the “old‑school” crew): diphenhydramine (Benadryl), chlorpheniramine, hydroxyzine.
- Second‑generation (the “new‑wave” squad): cetirizine (Zyrtec), loratadine (Claritin), fexofenadine (Allegra).
The main difference? First‑generations tend to make you feel a bit drowsy and cross the placenta more readily, while second‑generations usually keep you alert and still pass through the placenta, but in much lower amounts.
First vs. Second Generation
Both generations have been studied extensively, and—overall—they’ve earned a solid safety badge from regulatory agencies. Let’s break it down with a quick snapshot:
| Drug (Brand) | Generation | Pregnancy Category | Sedation? | Typical Use in Pregnancy |
|---|---|---|---|---|
| Diphenhydramine (Benadryl) | First | B | Yes | Allergy, nausea, sleep |
| Chlorpheniramine (Chlor‑Trimeton) | First | B | Moderate | Cold & allergy symptoms |
| Cetirizine (Zyrtec) | Second | B | Low | Seasonal allergies |
| Loratadine (Claritin) | Second | B | Low | Allergy & hives |
| Fexofenadine (Allegra) | Second | B | None | Allergy, urticaria |
| Cyproheptadine (Periactin) | First | C/D* | High | Appetite stimulant – avoid |
*Category C/D signals limited data or potential risk; it’s best to steer clear during pregnancy.
These categories aren’t just academic jargon. A 2008 review in Canadian Family Physician confirmed that first‑generation antihistamines have a long track record of safety, while newer studies on second‑generations, like the 2013 investigation in J Allergy Clin Immunol Pract, show reassuring outcomes for both mother and baby.
First Trimester Tips
The first three months are the “golden window” when organs are forming, so most expectant parents fret the most here. The biggest question is: “Will an antihistamine cause birth defects?” The short answer: the evidence doesn’t point to a heightened risk.
A systematic review titled “Antihistamine Use in Early Pregnancy and Risk of Birth Defects” examined hundreds of pregnancies and found no clear link between common antihistamines and major malformations (expert review of the literature). In plain language: you can generally breathe easier knowing that taking diphenhydramine or loratadine in the first trimester isn’t a red flag.
That said, a few practical pointers help you navigate this delicate phase:
- Start low, go slow. For cetirizine, 10 mg once a day is usually enough. If you need more, talk to your OB first.
- Avoid experimental or prescription‑only antihistamines that haven’t been studied in pregnancy.
- Steer clear of cyproheptadine—its appetite‑stimulating properties haven’t been vetted for early fetal development.
Later Pregnancy Advice
Once you’re past week 12, the baby’s architecture is largely set, and the focus shifts to growth and comfort. That’s when many pregnant people ask, “Can I keep using the same med, or should I switch?”
Both first‑ and second‑generation drugs remain acceptable. The deciding factor usually becomes side‑effects. If a first‑gen antihistamine makes you drowsy during the day, you might want to shift to a non‑sedating second‑gen option for a clearer head while you’re juggling prenatal appointments.
One nuance: some antihistamines can reduce uterine tone if taken in very high doses, though normal therapeutic doses are far below that threshold. So, stick to the labeled amount, and if you ever feel unusually dizzy or light‑headed, call your healthcare provider.
FAQs About Safety
Below are the quick‑fire questions most pregnant folks type into Google. Feel free to bookmark this section for a fast answer later.
Can I take Benadryl while pregnant?
Yes. Diphenhydramine (Benadryl) is a Category B antihistamine, meaning animal studies haven’t shown risk, and human data are reassuring. A typical dose is 25 mg every 6‑8 hours—no more than 150 mg in 24 hours. Keep it low, especially if you need it for night‑time relief.
Is loratadine safer than cetirizine?
Both are pegged as safe, and the difference comes down to personal tolerance. Some people feel a hint of drowsiness with cetirizine, while loratadine stays completely wakeful. Your choice can be guided by how you react to each on a non‑pregnant day.
What antihistamines should I avoid?
Beyond cyproheptadine, stay away from any drug that lacks a clear pregnancy classification (often newer, prescription‑only agents). If a medication is labeled “Category X” or “not studied in pregnancy,” give it a hard pass.
Do antihistamines get into breast milk?
Only in trace amounts. The same 2008 Canadian review noted that breastfeeding mothers can usually continue their antihistamine regimen without worrying about infant exposure.
Should I talk to my OB before taking any OTC allergy med?
Absolutely—especially if you’re on other prescriptions, have asthma, or have a chronic condition. A quick chat can prevent drug‑drug interactions and give you peace of mind.
Personal Experiences Shared
Stories are the spice of any health conversation. Here are a couple of real‑world snapshots (anonymized, of course):
I Had a Bad Rash at 10 Weeks
Emily (28 weeks pregnant) posted in a mom forum that a sudden eczema flare left her desperate. After a brief consult, her OB prescribed cetirizine 10 mg daily. She reported the rash cleared in a week, and she delivered a healthy baby. “I was nervous at first,” she wrote, “but the doctor explained the research, and I felt confident.”
Night‑time Itching in the Third Trimester
Jenna (36 weeks) struggled with relentless itching. She tried a low‑dose diphenhydramine (25 mg at bedtime) and slept through the night. The next morning, she felt a little groggy but said the rest‑of‑the‑day was itch‑free. She later switched to a non‑sedating loratadine for daytime use, keeping the night‑time diphenhydramine only when needed.
These anecdotes aren’t medical advice, but they illustrate how a thoughtful, doctor‑guided approach can keep symptoms under control without compromising safety.
How to Choose Safely
When you’re standing in the pharmacy aisle, the tiniest decision can feel enormous. Here’s a simple cheat‑sheet to help you pick the right antihistamine:
Check the label: “Pregnancy Category B”
Most reputable brands will list the FDA category on the back. If you can’t spot it, ask the pharmacist.
Start low, go slow
Begin with the lowest effective dose. For loratadine, that’s 10 mg once daily; for diphenhydramine, 25 mg at night.
Watch for side‑effects
Common: drowsiness (first‑gen), dry mouth, constipation. If anything feels off—especially dizziness or rapid heartbeat—call your provider.
Use a decision‑tree
1️⃣ How severe are your symptoms?
• Mild → saline rinse, humidifier → no med needed.
• Moderate‑Severe → move to step 2.
2️⃣ What trimester?
• First → prefer non‑sedating (loratadine, cetirizine).
• Later → any Category B ok, just monitor drowsiness.
3️⃣ Any other meds?
• If you’re on asthma inhalers or antidepressants, double‑check for interactions.
Following this flow can spare you the guesswork and keep you feeling in control.
Bottom Line & Next Steps
- Most antihistamines, especially those labeled Category B, are safe throughout pregnancy.
- Avoid cyproheptadine and any drug without clear pregnancy data.
- Second‑generation, non‑sedating options (cetirizine, loratadine, fexofenadine) work well for daytime relief.
- First‑generation agents (diphenhydramine, chlorpheniramine) are reliable for night‑time or nausea, but keep an eye on drowsiness.
- Always discuss your choice with your OB/midwife, especially if you’re taking other prescriptions.
Feeling a bit more confident about your allergy arsenal? Great! If you have any lingering doubts, a quick call to your healthcare team can turn uncertainty into certainty. And hey—if you’ve tried an antihistamine during pregnancy, share your experience in the comments. Your story could be the reassurance another mom needs.
Remember, every pregnancy is unique, and you deserve care that feels both safe and personalized. Here’s to clear sinuses, comfortable nights, and a healthy journey for you and your little miracle.




















Leave a Reply
You must be logged in to post a comment.