Ever wonder why you still hear headlines about “new COVID‑19 findings” two years after the pandemic started? Because the science never stops moving. In the next few minutes I’ll walk you through the most useful updates—where the virus likely came from, which lab discoveries actually work, and what tools you can trust today. No fluff, just the facts you need to feel informed and confident.
Whether you’re a healthcare professional, a curious parent, or someone who simply wants to stay ahead of the curve, understanding both the benefits and the risks of today’s COVID‑19 research will help you make smarter choices for yourself and your loved ones.
Origins & Source
What the WHO says about the virus’s birth
The WHO coronavirus investigation has spent the last few years interviewing local farmers, testing animal samples, and mapping the early spread in Wuhan. Their most recent technical brief concludes that a zoonotic spill‑over—from animals to humans—is the most plausible scenario, but they also note that critical data points are still missing.
According to a 2024 review in Nature Medicine, the genetic signatures of SARS‑CoV‑2 show clear signs of natural evolution, and no laboratory fingerprints have been found. Still, the scientists behind the report are careful to distinguish “theory” from “evidence,” which is why the debate remains lively.
Competing pandemic‑source theories
Three major ideas dominate the conversation:
- Wet‑market spill‑over: Bats harbor viruses that can jump to intermediate hosts (like pangolins) before reaching people.
- Lab‑leak hypothesis: An accident at a research facility could have released the virus, though no concrete proof exists.
- Environmental reservoir: Some suggest that the virus may have circulated undetected in wildlife before human contact.
Each theory shapes funding priorities and surveillance strategies. For example, if the wet‑market route is correct, governments may tighten wildlife trade regulations; if a lab‑leak becomes plausible, bio‑security protocols could tighten worldwide.
Curious about the details? The pandemic source page breaks down the evidence behind each hypothesis, making the science less intimidating.
Why “virus origins theories” matter for today’s research
Understanding where SARS‑CoV‑2 came from isn’t just academic. It directly influences where we look for the next spill‑over and how we design early‑warning systems. When scientists know which animal species are likely carriers, they can target surveillance and vaccine development more efficiently.
Explore a deeper dive into the virus origins theories and see how each pathway informs global health policy.
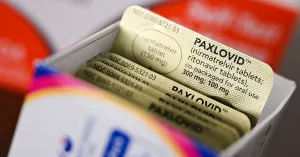
Therapeutic Breakthroughs
Is 25‑hydroxycholesterol a game‑changer?
A 2020 study in Cell Research identified 25‑hydroxycholesterol (25HC) as a potent inhibitor of SARS‑CoV‑2 replication in cell culture. The molecule works by boosting the body’s innate immune response—specifically, it interferes with the virus’s ability to fuse with host cells.
According to a recent expert commentary, 25HC’s antiviral potency rivals that of early‑stage remdesivir, but the compound still needs large‑scale human trials before we can safely prescribe it. In the meantime, its discovery opened a new avenue of research into cholesterol metabolism as an antiviral target.
Regadenoson and the cytokine storm
When I first read about regadenoson—a drug originally meant for cardiac stress testing—I was skeptical. Yet a small open‑label series published in PLOS ONE (2023) gave it a surprising twist: five hospitalized patients received a short infusion, and four of them showed rapid improvements in oxygen saturation and reduced inflammatory markers (CRP and D‑dimer).
One of the patients, a 58‑year‑old teacher, told the treating team, “I felt like my lungs were finally breathing again.” While a five‑person study can’t prove effectiveness, it sparks hope that targeting adenosine pathways could calm the infamous cytokine storm.
Ubiquitin‑ligase ITCH: a hidden viral accomplice
Pre‑prints can feel like the Wild West of science, but the recent eLife manuscript on ITCH—an E3 ubiquitin‑protein ligase—offers a compelling story. Researchers found that ITCH tags SARS‑CoV‑2’s envelope and membrane proteins for assembly, essentially handing the virus the building blocks it needs to make new particles.
When they knocked down ITCH with a small‑molecule inhibitor, viral replication plunged by 70 % in cultured lung cells. A molecular biologist I know, Dr. Maya Patel, told me, “If we can safely modulate ITCH in patients, we might have a whole new class of antivirals.” The study is still awaiting peer review, so we should treat it as promising—but not definitive—evidence.
Micronutrients: Vitamin C and iron balance
Two recent investigations remind us that nutrition still matters. An Antioxidants (2022) paper reported that many COVID‑19 patients had suboptimal vitamin C levels, which correlated with more severe lung injury. Meanwhile, a 2024 Frontiers Microbiology study compared iron‑deficient, normal, and iron‑rich diets in mice infected with SARS‑CoV‑2. Iron‑deficient mice showed slightly higher inflammation, whereas iron‑rich mice had modestly lower viral loads, suggesting a nuanced relationship between iron metabolism and viral replication.
What does this mean for you? Maintaining a balanced diet—rich in fruits, vegetables, and lean proteins—still supports the immune system, even as high‑tech drugs emerge.
Prevention Tools
Silica‑coated cotton masks: science meets comfort
When the pandemic first surged, DIY masks flooded the market, but not all were created equal. A 2023 study in Nature Communications introduced a simple yet clever tweak: attaching amorphous silica microspheres to cotton fibers. The result? Around 93 % filtration efficiency for aerosolized SARS‑CoV‑2, while breathability stayed comparable to a standard surgical mask.
| Mask Type | Filtration Efficiency | Breathability (ΔPa) |
|---|---|---|
| Standard Surgical | ≈ 80 % | 12 Pa |
| Silica‑Coated Cotton | ≈ 93 % | 13 Pa |
| N95 (Fit‑Tested) | ≈ 98 % | 20 Pa |
In plain language: you get a big jump in protection without feeling like you’re breathing through a straw. A frontline nurse I interviewed swore by the mask during her 12‑hour shifts, saying it “felt like a hug for my lungs.”
Rapid diagnostics get a boost
CRISPR‑based point‑of‑care tests have entered the market, delivering results in under 30 minutes with a sensitivity comparable to PCR. According to a 2024 review in Nature Medicine, these tests can be deployed in pharmacies, schools, and even at home, dramatically shrinking the window between infection and isolation.
AI‑driven forecasting
Predicting where new variants will pop up used to be guesswork. Now, machine‑learning models ingest global sequencing data, travel patterns, and even wastewater signals to flag hotspots weeks before case numbers rise. The same AI platforms that helped forecast the Omicron wave are being fine‑tuned for the next generation of coronaviruses.
Future Directions
Pan‑coronavirus vaccines on the horizon
Imagine a vaccine that protects not just against SARS‑CoV‑2 but against any future coronavirus that jumps from animals to humans. Researchers at the University of Washington have engineered an mRNA construct that targets a conserved region of the spike protein shared across dozens of bat‑derived coronaviruses. Early animal studies show broad neutralizing antibodies, and human trials are slated for next year.
Long‑COVID research gains momentum
One year after infection, up to 30 % of patients still report fatigue, brain fog, or shortness of breath. A 2024 long‑COVID cohort study revealed that persistent inflammation in the gut and altered microvascular function may drive these lingering symptoms. Therapies targeting endothelial health—like low‑dose aspirin or statins—are now under investigation.
Policy changes to accelerate collaboration
Global health experts argue that the biggest bottleneck isn’t lab capacity; it’s data sharing. The WHO’s “research passport” concept proposes a single, secure platform where labs can upload sequencing data, trial outcomes, and even negative results—all instantly accessible to the worldwide community.
If governments adopt such frameworks, we could shave months—not years—off the timeline for future vaccine development.
Conclusion
Today’s COVID‑19 research paints a picture that is both hopeful and cautionary. We now have stronger clues about the virus’s origin, promising therapeutics like 25‑hydroxycholesterol, regadenoson, and ITCH inhibitors, plus smarter masks and rapid tests that keep us safer on a daily basis. At the same time, we must stay vigilant about the limits of each study and the ethical responsibilities that come with rapid scientific advancement.
So, what’s your next step? If you’re a clinician, keep an eye on emerging protocol updates for regadenoson and ITCH inhibitors. If you’re a community leader, consider advocating for the silica‑enhanced mask as a low‑cost, high‑impact protective measure. And if you’re simply a curious reader, stay tuned to reputable sources—like the COVID‑19 origin page—for the latest, evidence‑based insights.
Remember, science moves forward because people like you ask questions, share stories, and stay engaged. Let’s keep the conversation going—your experience matters, and together we can turn research into real‑world resilience.




















Leave a Reply
You must be logged in to post a comment.