Hey there! If you’ve ever felt that sudden woozy spell or that spinning sensation that makes you think the world’s doing a pirouette, you’re not alone. Dizziness is one of those pesky symptoms that pops up when you least expect it, and figuring out why can feel like solving a mystery on a rainy night. Below, I’ll walk you through the most common dizziness causes, show you how to recognize them, and share practical ways to stop dizziness before it ruins your day. Grab a cup of tea, settle in, and let’s untangle this together.
Quick Answer
What is dizziness? It’s a blanket term for feelings of light‑headedness, unsteadiness, or the sensation that you or your surroundings are spinning. The three biggest culprits? Inner‑ear problems, reduced blood flow to the brain, and medication or health‑condition side‑effects.
Why It Matters
Knowing the cause isn’t just trivia—it can protect you from falls, prevent unnecessary doctor visits, and help you get the right treatment faster. When you understand the “why,” you can decide whether a simple home remedy will do, or if it’s time to call in a specialist. Plus, the peace of mind that comes from a clear explanation is priceless.
Major Categories
Inner‑Ear (Peripheral Vestibular) Issues
The inner ear houses tiny structures that act like gyroscopes, constantly sending balance signals to your brain. When they go wonky, dizziness follows.
Benign Paroxysmal Positional Vertigo (BPPV)
This is the most common vestibular problem. Tiny calcium crystals (otoconia) drift into one of the semicircular canals, sending false “I’m moving” messages whenever you tilt your head. You’ll feel a brief, intense spin—often when you roll over in bed or look up.
Meniere’s Disease
Think of your inner ear as a tiny aquarium. When excess fluid builds up, it creates sudden, prolonged episodes of vertigo that can last minutes to hours, often paired with ringing in the ears (tinnitus) and muffled hearing.
Vestibular Neuritis / Labyrinthitis
These are viral inflammations of the vestibular nerve or the labyrinthine structures. The dizziness tends to be constant for days, sometimes with nausea, but without hearing loss.
Acoustic Neuroma
Although rare, a benign tumor on the vestibular nerve can cause progressive unsteadiness, unilateral hearing loss, and tinnitus. If you notice these symptoms slowly worsening, it’s worth a specialist’s look.
Reduced Blood Flow & Cardiovascular Causes
Your brain is a high‑maintenance organ—if it doesn’t get enough blood, it throws a wobble party.
Arteriosclerosis / Atherosclerosis
Hardening of the arteries can limit blood to the brain, especially in the vertebrobasilar system that supplies balance centers. Dizziness may come on gradually or after exertion.
Anemia & Low Blood Sugar
Both conditions starve the brain of oxygen or glucose. You might feel light‑headed after skipping a meal or during a heavy period.
Dehydration & Overheating
When you lose fluids, blood volume drops, and you can feel faint, especially when standing up quickly.
Orthostatic Hypotension
This is a sudden blood‑pressure dip when you move from lying down to standing. Medications for high blood pressure, heart disease, or even certain antidepressants can trigger it.
Medication & Substance‑Induced Dizziness
Every pill has a side‑effect profile, and many include dizziness.
- Blood‑pressure meds (especially diuretics)
- Antidepressants and anti‑seizure drugs
- Antihistamines, sleep aids, and some antibiotics
- Alcohol, caffeine, or nicotine withdrawal
If you’ve started a new medication and feel off‑balance, double‑check the label or ask your pharmacist. A quick dosage tweak can make all the difference.
Systemic & Neurologic Conditions
Sometimes the cause lies deeper than the ear or the heart.
Migraine‑Associated Vertigo
Even without a pounding headache, migraines can cause spinning sensations, sensitivity to light, and nausea. The episodes may last from minutes to days.
Multiple Sclerosis
When demyelination hits the brainstem or cerebellum, balance pathways get disrupted, leading to intermittent dizziness.
Stroke or Transient Ischemic Attack (TIA)
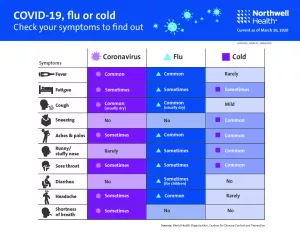
A sudden, severe dizziness with vision changes, slurred speech, or facial weakness is a red‑flag. According to Mayo Clinic, this warrants emergency care.
Psychogenic Dizziness
Anxiety, panic attacks, or chronic stress can produce a “floaty” feeling. While the sensation is real, the underlying cause is emotional rather than structural.
Diagnosis Steps
| Step | What to Do | Who Helps |
|---|---|---|
| 1️⃣ Symptom Diary | Write down when dizziness occurs, triggers, duration, and any accompanying symptoms (nausea, hearing changes, vision blur). | You |
| 2️⃣ Physical Exam | Vitals, orthostatic blood pressure, Dix‑Hallpike maneuver, head‑impulse test. | Primary‑care or ENT |
| 3️⃣ Basic Labs | CBC, blood glucose, electrolytes, thyroid panel. | Lab technician |
| 4️⃣ Imaging (if needed) | MRI of brain or CT angiography to rule out stroke, tumor, or inner‑ear abnormalities. | Radiology |
| 5️⃣ Specialist Referral | ENT/vestibular therapist, cardiologist, neurologist, or mental‑health professional. | Physician |
These steps not only pinpoint the cause but also reassure you that nothing is being overlooked. A clear roadmap is the best way to feel in control.
Stop Dizziness
At‑Home First‑Aid
When a dizzy spell hits, the first thing to do is sit or lie down—preferably with your head slightly elevated. Sip water, turn on a fan if you feel overheated, and focus on breathing slowly. For BPPV, the Epley maneuver can often reset those rogue crystals within minutes.
Lifestyle Adjustments
- Hydrate. Aim for 2‑3 liters of water daily, more if you’re active or live in a hot climate.
- Eat balanced meals. Iron‑rich foods (spinach, lentils) and B‑vitamins support blood oxygenation.
- Move slowly. When getting up from bed or a chair, pause for a few seconds to let your circulation adjust.
- Exercise. Gentle balance training—think Tai Chi or yoga—strengthens the vestibular system.
- Limit alcohol & caffeine. Both can dehydrate you and spike blood pressure fluctuations.
When Medication Helps
Short‑term vestibular suppressants like meclizine or dimenhydrinate can calm awful spins, but they’re not a long‑term fix. Treat the root cause—whether that’s adjusting blood‑pressure meds, starting migraine prophylaxis, or beginning a vestibular rehabilitation program.
Red‑Flag Situations
If you notice any of the following, seek medical attention right away:
- Sudden, severe dizziness with double vision, slurred speech, or facial weakness.
- Persistent vomiting that prevents you from keeping fluids down.
- Sudden hearing loss or ringing in one ear.
- Fainting or loss of consciousness.
- Dizziness after a head injury.
These symptoms could signal a stroke, inner‑ear infection, or other serious conditions.
Resources & Trustworthy References
For deeper dives, the following sources keep their information up‑to‑date and evidence‑based:
- Mayo Clinic – Dizziness Causes
- American Vestibular Society – Causes of Dizziness
- WebMD – Dizziness Overview
- Healthline – Sudden Dizziness and Nausea
Conclusion
Dizziness can stem from the inner ear, the circulatory system, medications, or deeper neurologic issues. By tracking your symptoms, getting a focused exam, and acting on the right treatment, most people can find relief and prevent complications. If any red‑flag signs appear, don’t wait—seek care right away. Stay informed, stay safe, and don’t let dizziness hold you back.
Got a story about a dizzy moment that turned out to have an unexpected cause? Share it in the comments below—your experience might help someone else figure out theirs. And if you found this guide useful, feel free to bookmark it for the next time you feel a little “off‑balance.”





















Leave a Reply
You must be logged in to post a comment.