If you or someone you love lives with Parkinson’s, you’ve probably heard doctors talk about “tremor tests” or “motor exams.” What if I told you that a tiny, everyday motion—just tapping your thumb and index finger together—can reveal hidden changes in the disease — sometimes even before a tremor becomes obvious? In the next few minutes I’ll walk you through exactly what the finger‑tapping test measures, why clinicians rely on it, how new technology makes it sharper, and how you can use the results to keep your treatment plan on point. Grab a cup of tea, settle in, and let’s explore this surprisingly powerful tool together.
What Is The Test?
Definition & Core Purpose
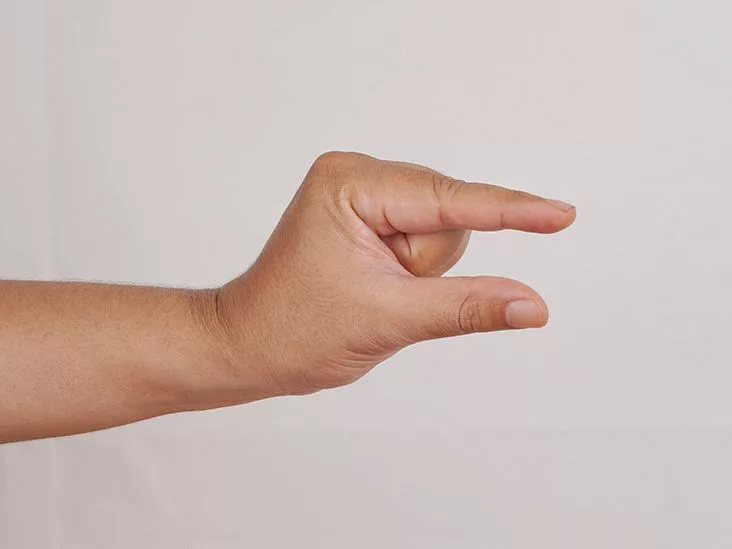
The finger‑tapping test is a simple clinical maneuver that examines bradykinesia—the hallmark slowness of movement in Parkinson’s. By asking a person to tap the thumb and index finger together as quickly and as widely as possible, a doctor can watch four key features:
- Speed (how many taps per second)
- Amplitude (how far the finger moves)
- Rhythm (how regular the taps are)
- Fatigue (whether performance drops over a few seconds)
All of these clues help map the subtle motor‑symptom landscape that standard tremor tests might miss.
Historical & Scientific Background
The test has been a staple of the Unified Parkinson’s Disease Rating Scale (UPDRS) for decades, providing a quick window into basal‑ganglia function. According to Healthline, even a tiny reduction in tapping speed can signal disease progression before visible shaking appears.
Quick‑Look Comparison Table
| Feature | Traditional Clinician Observation | Smartphone‑Sensor Version |
|---|---|---|
| Objectivity | Subjective visual rating | Millisecond‑level timestamps |
| Setting | In‑office only | Home‑monitoring possible |
| Cost | Minimal (pen & paper) | Low‑to‑moderate (app/device) |
How It Evaluates Symptoms
Speed & Frequency
Healthy adults typically tap 7‑9 times per second. In early Parkinson’s you might see numbers dip to 4‑5 taps/sec, and the decline can become steeper as the disease advances.
Amplitude & “Height” of Taps
Amplitude is measured in millimetres or, more simply, by how far the thumb and index finger separate. A research article in the Movement Disorders Clinical Practice journal describes a “TAP score” that combines speed and height to give a single number clinicians can track over time.
Rhythm & Variability
When the taps become uneven—some fast, some slow—the rhythm coefficient of variation rises. A study published in BMJ Neurology found that Parkinson’s patients with cognitive impairment (PD‑CI) show significantly less rhythmic tapping than those with normal cognition (PD‑NC)【BMJ Neurology Below is a simple template you can print out. Record taps for each hand, note any pauses, and calculate a basic score (taps ÷ seconds). Over weeks, the trend speaks louder than any single number. 1. Non‑invasive & fast—under 30 seconds. While the test is safe, it isn’t a stand‑alone diagnosis. Results can vary if a patient is distracted, fatigued, or doesn’t understand the instructions. Without digital assistance, two clinicians might rate the same performance differently—a classic case of inter‑rater variability. “Finger‑tapping provides a window into basal‑ganglia function that we can watch over time,” says Dr. Marina Picillo, movement‑disorder specialist at Toronto Western Hospital. Companies like ClearSky have built the PD‑Monitor, which uses the phone’s camera to capture tap intervals, amplitude, and hesitation. According to a recent study, the device differentiated Parkinson’s from essential tremor with 94 % specificity and 92 % accuracy【ClearSky MD Dedicated electromagnetic or inertial sensors strapped to the hand can detect micro‑movements beyond the eye’s reach. These gadgets feed data into dashboards that display speed curves, amplitude trends, and fatigue indices. For folks living far from a specialist center, a simple tap recorded on a phone can be uploaded securely, allowing neurologists to adjust medication without an in‑person visit. The data‑driven feedback loop makes disease monitoring feel less like a guessing game.Sample Scoring Sheet (PDF placeholder)
Benefits vs Risks
Benefits (Why Clinicians Love It)
2. Quantifiable—gives numbers you can chart.
3. Early detection—tiny changes often appear before tremor intensifies.
4. Medication monitoring—helps pinpoint “on/off” periods after levodopa.Risks & Limitations (A Balanced View)
Expert Quote
Digital & AI Tools
Smartphone & Tablet Apps
Wearable Sensors
Remote Monitoring & Tele‑Neurology
Comparison Matrix
| Feature | Hand‑Held App | Dedicated Sensor |
|---|---|---|
| Accuracy | Good (camera‑based) | Excellent (millimetre precision) |
| Cost | Low (free or $) | Moderate‑High (device purchase) |
| Ease of Use | Very easy | Requires set‑up |
| Remote Capability | Instant upload | Bluetooth sync |
Integrating Into Assessment
When To Perform It
Most neurologists do the test at every routine visit—usually before medication is taken and again 30‑45 minutes after the dose. For home‑based tracking, a weekly tap session (same time of day, same posture) creates a reliable baseline.
How Clinicians Record & Interpret
Results are entered into the UPDRS Part III (Motor Examination) and plotted on a longitudinal chart. A steady decline in taps per second may prompt a medication tweak; an improvement could confirm that a new dose is effective.
Linking to Medication Management
Imagine you notice a 15 % drop in tap speed right before your evening levodopa wears off. Your neurologist can adjust the timing or add a short‑acting formulation, turning that brief dip into a smoother “on” period.
Patient‑Care Pathway Flowchart (placeholder)
1️⃣ Baseline test → 2️⃣ Record data → 3️⃣ Review at visit → 4️⃣ Adjust meds → 5️⃣ Repeat. Simple, repeatable, and data‑rich.
Real‑World Case Studies
Case A – Early‑Stage Detection
John, 58, was diagnosed with Parkinson’s two years ago. At his first visit his tap rate was 6.8 taps/sec. Six months later, despite feeling “fine,” his rate slipped to 5.2 taps/sec. The neurologist increased his levodopa dose, and a follow‑up showed the tap rate rebound to 6.5 taps/sec. The early numeric cue saved John from a silent decline.
Case B – Differentiating From Essential Tremor
Maria, 62, presented with a shaky hand but no obvious bradykinesia. Using the PD‑Monitor, clinicians recorded her tapping pattern. The AI‑classifier flagged a high specificity profile for essential tremor, not Parkinson’s. She avoided unnecessary dopaminergic medication and was instead referred for physiotherapy targeting tremor control.
Patient Voice (anonymous)
“Seeing my tap numbers on a graph gave me something concrete to discuss with my doctor. It felt empowering, not scary.”
Step‑By‑Step Guide
Preparation
- Sit comfortably at a table, elbow rested.
- Remove rings or bulky jewelry.
- Place the hand flat, palm down.
Execution (per hand)
- Explain: “Tap your thumb and index finger together as fast and as wide as you can.”
- Set a timer for 15 seconds (most clinicians use 10‑15 seconds).
- Start tapping. Count out loud or let a phone video capture the motion.
- When time’s up, stop and note the total taps.
Recording & Analysis
If you’re using a simple stopwatch, write the count in a notebook and divide by 15 seconds to get taps per second. With an app, the software will automatically generate speed, amplitude, and rhythm graphs.
Troubleshooting Checklist
- Patient hesitates? Encourage a “just try, no pressure.”
- Hand shakes excessively? Note the tremor but focus on tap speed.
- Fatigue appears after 8 seconds? Record the drop; it’s clinically relevant.
Personalized Monitoring Plan
Choosing the Right Tool
Consider your comfort with technology, budget, and what your neurologist recommends. A free smartphone app may be perfect for casual weekly checks; a dedicated sensor might be worth it if you’re in a clinical trial or need the highest precision.
Setting Alerts & Sharing Data
Most digital platforms let you set thresholds—e.g., “Alert me if tap speed drops 20 % from baseline.” The data can be shared securely with your care team via a cloud portal, ensuring your doctor sees real‑time trends.
Weekly Log Template (downloadable)
Day | Time | Hand | Taps/15 sec | Notes (fatigue, meds) — keep it simple, but consistency is key.
Sources & Further Reading
For those who love to dig deeper, the following resources underpin the information in this article:
- Healthline – “How Is Finger Tapping Used In Parkinson’s Disease?”
- NCBI – Learning More from Finger Tapping in Parkinson’s Disease: Up and Down from Dyskinesia to Bradykinesia (2015)
- BMJ Neurology – “Finger Tapping and Cognition in Parkinson’s” (2015)
- ClearSky MD – Study on differentiating Parkinson’s from essential tremor using finger tapping
Conclusion
The finger‑tapping test may look like a child’s game, but in the hands of a neurologist (or a savvy patient with a smartphone) it becomes a powerful mirror of the brain’s motor pathways. It catches subtle slow‑downs, guides medication tweaks, and—thanks to AI‑enabled apps—lets you track your own progress from the comfort of home. So the next time your doctor asks you to tap your thumb and index finger, remember: you’re not just tapping for fun; you’re gathering data that could keep your treatment tighter, your symptoms steadier, and your quality of life higher.
Give it a try this week, jot down the numbers, and share the trend with your care team. If you have questions or want to swap experiences, feel free to leave a comment below. Let’s keep the conversation going—because together we can make Parkinson’s monitoring a little less mysterious and a lot more empowering.























Leave a Reply
You must be logged in to post a comment.