Imagine watching a loved one battle cirrhosis—watching their energy fade, seeing medication bottles pile up, and feeling the weight of “what’s next?” You’re not alone. Many families hit that crossroads where a liver transplant feels like the only beacon of hope. The good news? A living‑donor or partial liver transplant can be a lifeline, and it’s more doable than you might think. Let’s walk through everything you need to know about liver donation cirrhosis—from why it’s needed, to who can donate, to the real‑world risks and rewards—all in a friendly, conversational style.
Cirrhosis and Transplant Need
What Is Cirrhosis?
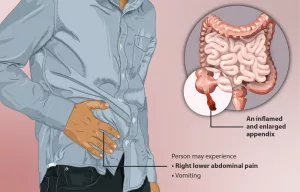
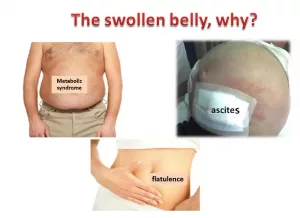
Cirrhosis is the scar‑filled version of liver disease. Healthy liver tissue gets replaced by tough, fibrous tissue, and the organ can’t perform its >400 essential jobs—producing bile, detoxifying blood, clotting proteins, and storing nutrients. When those jobs start slipping, you get symptoms like fatigue, abdominal swelling (ascites), and confusion (hepatic encephalopathy). MedlinePlus explains cirrhosis in plain language, and it’s a perfect reminder that the liver isn’t just a “fat storage tank”; it’s the body’s busy multitasker.
Why Does Cirrhosis Often Lead to a Transplant?
Medical therapies can slow progression, but they can’t reverse scarring. When the disease reaches a decompensated stage—meaning the liver can’t keep up—the Cleveland Clinic notes that a transplant becomes the definitive treatment. Doctors use MELD (Model for End‑Stage Liver Disease) scores to decide who’s in the most urgent need; a high MELD score usually signals that a transplant is the only viable option.
When Is Transplant Recommended?
- Recurrent ascites that won’t respond to diuretics.
- Frequent hepatic encephalopathy episodes.
- Life‑threatening variceal bleeding.
- Persistent jaundice or severe liver failure.
If any of these sound familiar in your family’s story, it’s time to talk with a transplant center about options—including a living‑donor liver transplant.
Living‑Donor Liver Transplant
How a Partial Liver Transplant Works
Here’s the magic: the liver can regenerate. A donor can give roughly 30‑45 % of their liver, and both the donor’s remaining piece and the recipient’s new piece grow back to full size within weeks. MedlinePlus describes the process, emphasizing that the organ’s regenerative ability is what makes living donation possible.
Who Can Be a Donor?
Not everyone qualifies, but the pool is broader than you might think. Typical criteria (as listed by Johns Hopkins Medicine) include:
- Age 18‑60.
- Body‑mass index (BMI) < 35.
- Compatible blood type with the recipient.
- Excellent overall health—no major heart, kidney, or lung disease.
- No active infections, malignancies, or chronic hepatitis.
- Strong psychosocial support system.
What the Recipient Gains
Living‑donor transplants cut wait times dramatically. Because the donor is scheduled ahead of time, the graft is fresh, reducing “cold‑ischemia time” (the period the organ is without blood). Fresh grafts mean fewer complications and better long‑term survival. Cleveland Clinic outlines these benefits in a clear, patient‑focused guide.
Donation Eligibility Process
Medical Screening Checklist
Before you even step into the operating room, a battery of tests will confirm your liver’s health and your body’s ability to safely donate. Expect:
- Comprehensive blood work (liver enzymes, hepatitis panels, coagulation studies).
- Imaging (CT or MRI to map liver volume).
- Cardiac evaluation (EKG, stress test).
- Kidney function tests.
- Volumetric analysis to ensure the donor’s remaining liver will be >30 % of original size.
Psychosocial Assessment
Donating isn’t just a physical decision; it’s emotional, too. A psychologist or social worker will explore your motivations, ensure there’s no coercion, and verify you have a solid support network for recovery. The process respects autonomy—donors must give fully informed, voluntary consent.
Legal & Ethical Safeguards
Federal law prohibits any form of payment for organs. All living‑donor programs follow strict ethical guidelines, including donor anonymity options if desired. Documentation of consent, counseling records, and a clear statement that you’re not under pressure are all part of the legal safety net.
Eligibility Table
| Criteria | Eligible | Ineligible |
|---|---|---|
| Age | 18‑60 | <18 or >60 |
| BMI | <35 | ≥35 |
| Blood Type | Compatible with recipient | Incompatible |
| Organ Health | No major heart, kidney, lung disease | Significant organ disease |
| Infections | Negative for active hepatitis, HIV, etc. | Active infection or chronic hepatitis |
| Psychosocial | Strong support, no coercion | Substance abuse, mental health instability |
Donor Benefits and Risks
Potential Benefits for the Recipient
The most obvious win is a life‑saving organ, but there’s more:
- Higher survival rates (over 85 % 5‑year survival).
- Shorter hospital stay because the graft is fresh.
- Reduced risk of rejection thanks to a better‑matched, healthier organ.
Short‑Term Risks to the Donor
Any major surgery carries risks. For living‑donor liver surgery, data from large multicenter studies (a 2023 review in Transplantation) show:
- Major complications in <1 % of donors (bleeding, bile leak, infection).
- Minor complications (pain, wound infection) in about 10 %.
- Mortality around 0.3 %—still low but not zero.
Recovery usually means a 5‑7‑day hospital stay, followed by two weeks of limited activity. Most donors feel “back to normal” within 4‑6 weeks.
Long‑Term Donor Outcomes
Over 95 % of donors enjoy complete liver regeneration with no lasting functional deficits. A tiny fraction develop chronic liver disease later—often linked to unrelated factors like alcohol use or hepatitis infection, not the donation itself.
Risk‑vs‑Benefit Matrix
| Aspect | Benefit | Risk |
|---|---|---|
| Recipient Survival | 85 %+ 5‑year survival | None (benefit only) |
| Donor Recovery | Regeneration in 6‑8 weeks | ~10 % minor complications |
| Surgical Mortality | Life saved for recipient | 0.3 % donor mortality |
| Emotional Impact | Deep personal fulfillment | Potential guilt if graft fails |
Partial Liver Transplant Steps
Pre‑Op Planning
The journey starts months before the scalpel touches skin. A multidisciplinary team—surgeon, hepatologist, anesthesiologist, radiologist, psychologist—will map out the donor‑recipient match using 3‑D imaging. This ensures the donor’s right lobe (or left, depending on size) will be sufficient for the recipient.
Surgery Day Timeline
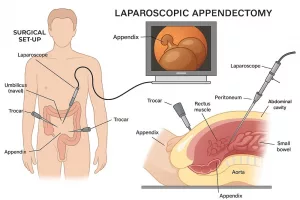
- Morning: Both donor and recipient enter separate ORs for parallel preparation.
- Donor Hepatectomy: Surgeons remove the chosen liver segment, preserving vascular and bile ducts.
- Cold Preservation: The graft is flushed with a cold preservation solution and transported on ice (usually under 8 hours).
- Recipient Implantation: The graft is sewn into place, blood vessels and bile ducts are reconnected.
- Reperfusion: Blood flow resumes—often a dramatic moment where the new liver “wakes up.”
- Closure & Transfer: Donor and recipient move to ICU for monitoring.
Post‑Op Care for Donor
Donors spend 24‑48 hours in the ICU for vital‑sign monitoring, liver‑function labs, and pain control. Most are discharged by day 5‑7. Instructions include:
- Limited lifting (no >10 lb) for 4‑6 weeks.
- Follow‑up imaging at 1 month to confirm liver growth.
- Balanced diet rich in protein to aid regeneration.
Post‑Op Care for Recipient
Recipients remain in the ICU for a few days, then move to a transplant floor. Immunosuppressive meds (tacrolimus, steroids) are started to prevent rejection. Lab checks (AST, ALT, bilirubin) are done daily for the first week. Most leave the hospital within 2‑3 weeks, assuming no complications.
Recovery and Long‑Term Outlook
Donor Recovery Milestones
Here’s a quick timeline to keep you motivated:
- Week 1: Pain manageable, light walking.
- Week 2: Liver volume ~50 % of original size.
- Weeks 4‑6: Most daily activities feel normal.
- Weeks 6‑8: Full‑size regeneration; labs back to baseline.
Recipient Milestones
The recipient’s journey is a bit more variable, but typical checkpoints include:
- Day 2‑3: Graft function starts improving (bilirubin drops).
- Week 1‑2: ICU discharge, start gentle physiotherapy.
- Month 1‑3: Gradual reduction of steroids, stable imaging.
- Year 1: Most enjoy a near‑normal lifestyle with routine labs.
Support Resources
Both donors and recipients benefit from peer groups, counseling, and educational toolkits. The American Liver Foundation offers a downloadable toolkit, and the Donate Life Living‑Donor Registry helps you connect with transplant centers.
Getting Started Resources
Official Donor Registries
If you feel called to donate, start by registering with your national donor program. In the U.S., the National Donate Life Living‑Donor Registry is a secure, free way to indicate your willingness.
Educational Portals
- American Liver Foundation – Living‑Donor Liver Transplant Information Center.
- Cleveland Clinic – Detailed guides for donors and recipients.
- MedlinePlus – Easy‑to‑read medical overviews.
Contact Your Transplant Center
When you reach out, bring these questions:
- What’s the typical timeline from evaluation to surgery?
- What support services are offered during recovery?
- How are potential complications managed?
Take the First Step
Even if you’re just gathering information, the act of learning is powerful. Write down what you’ve discovered, share it with your family, and consider a preliminary medical check‑up. You never know—what starts as curiosity could become a life‑changing decision for someone you love.
At the end of the day, the choice to donate a part of your liver is deeply personal. It’s also a testament to the incredible resilience of the human body—and the extraordinary compassion we can show one another. If you’re standing at that crossroads, remember you’re not walking it alone. Reach out, ask questions, and let the expertise of transplant teams guide you. Your willingness to explore liver donation for cirrhosis already shines a light for those who need it most.





















Leave a Reply
You must be logged in to post a comment.