Hey there! If you’ve ever wondered why your doctor keeps mentioning “metabolic syndrome” or why a simple waist measurement feels like a secret code, you’re in the right spot. In the next few minutes we’ll break down the most important metabolic syndrome indicators, peek at some cutting‑edge gut‑health clues, and give you a game plan you can actually use. No fluff, no jargon—just clear, friendly advice you can act on right now.
What Is Metabolic Syndrome
Simple definition in plain language
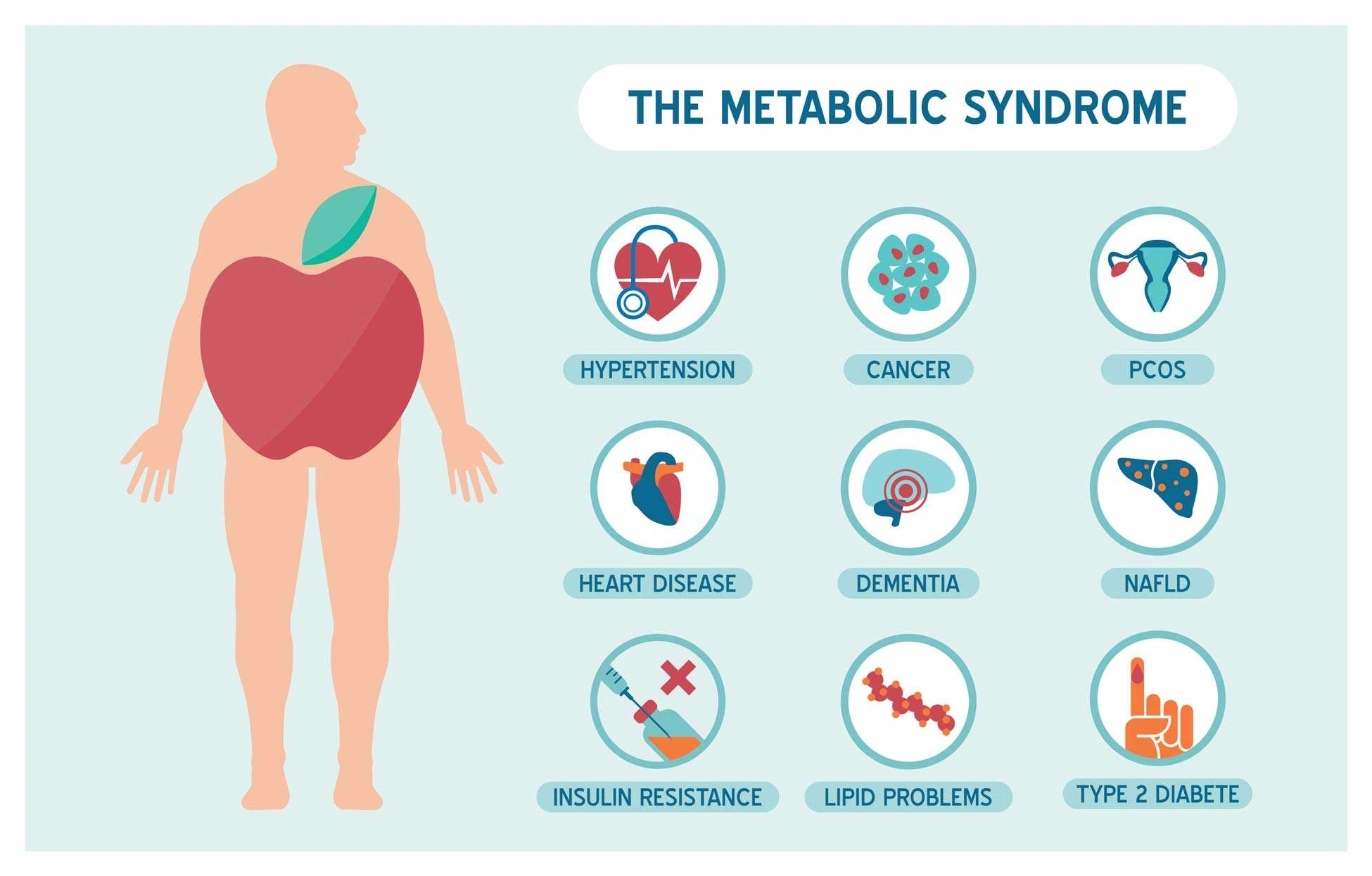
Think of metabolic syndrome as a “danger package” of five health factors that, when they show up together, dramatically raise your chances of heart disease, stroke, and type 2 diabetes. The package includes:
- Abdominal obesity (big waistline)
- High blood pressure
- Elevated fasting blood sugar
- High triglycerides
- Low “good” HDL cholesterol
When three or more of these line up, the label “metabolic syndrome” gets stuck on your chart.
How the five risk factors combine
Each factor alone is a warning sign, but together they act like a multiplier. For example, high blood pressure alone raises heart‑attack risk by about 2‑fold; add a big waist and high blood sugar and that risk can jump to 5‑fold or more. According to the National Heart, Lung, and Blood Institute (NHLBI), the synergy of these markers is what makes metabolic syndrome such a serious health concern.
Who is most likely to develop it?
Age, genetics, and lifestyle all play a role. The risk climbs after age 40, is higher in certain ethnic groups (e.g., African‑American women), and is strongly linked to being overweight. But the good news? Lifestyle tweaks can turn the tide for most people.
Core Clinical Indicators
Abdominal obesity – waist circumference thresholds
Measure around the narrowest part of your torso, or right above the hip bones if your waist tapers. The cut‑offs are:
| Group | Men | Women |
|---|---|---|
| Standard threshold | > 40 in (102 cm) | > 35 in (89 cm) |
| Asian‑specific | > 35 in (89 cm) | > 30 in (76 cm) |
Even a few extra inches can signal the start of the “danger package.” If you’re curious how your gut might be influencing waist size, check out our article on digestive health for practical tips.
Elevated blood pressure (≥ 130/85 mm Hg)
High blood pressure often feels invisible—no pain, no obvious symptoms—yet it’s a major player. A quick home cuff reading above 130 systolic or 85 diastolic should prompt a doctor’s visit. Chronic hypertension can damage artery walls, making them “sticky” for cholesterol plaques.
High fasting glucose (100‑125 mg/dL) and pre‑diabetes
When you fast for at least 8 hours and your blood sugar lands between 100 and 125 mg/dL, you’re in the pre‑diabetes zone. Symptoms, if they appear, can include extra thirst, frequent bathroom trips, and occasional fatigue. If you notice any of these, ask your provider for an HbA1c test—it gives a longer‑term picture of glucose control.
High triglycerides (≥ 150 mg/dL)
Triglycerides are the fat you get from excess calories, especially carbs and alcohol. Levels over 150 mg/dL are a red flag. Cutting sugary drinks, swapping refined carbs for whole grains, and adding omega‑3 rich foods (like salmon or chia seeds) can bring those numbers down.
Low HDL cholesterol (men < 40 mg/dL; women < 50 mg/dL)
HDL is the “good” cholesterol that helps sweep away the “bad” LDL. If you’re below the thresholds, lifestyle changes—regular aerobic exercise and healthy fats (olive oil, nuts)—are the first line of defense.
Emerging GI‑Tract Biomarkers
What are GI‑tract biomarkers?
Beyond the classic blood tests, researchers are uncovering gut‑derived markers that whisper early warnings about metabolic trouble. These include calprotectin (a sign of intestinal inflammation), zonulin (a marker of gut‑wall permeability), and lipopolysaccharide (LPS), which can trigger systemic inflammation when it leaks into the bloodstream.
Key inflammation biomarkers detectable in stool or blood
| Biomarker | What it tells us | Typical testing method |
|---|---|---|
| Calprotectin | Intestinal inflammation | Stool ELISA |
| Zonulin | Gut permeability (“leaky gut”) | Blood or stool assay |
| LPS | Systemic endotoxin load | Blood assay |
These markers don’t replace traditional panels, but they can help explain why someone with a “normal” lipid profile still struggles with weight gain or insulin resistance.
Gut microbiome’s influence on triglycerides & HDL
Recent studies (2024) show that certain gut bacteria produce short‑chain fatty acids that improve HDL levels and lower triglycerides. In other words, a happy gut can help clean up the blood‑fat mess. Want to see how to monitor your gut health? Our guide on gut health monitoring walks you through simple at‑home tests and diet tweaks.
When to order GI‑specific tests
Consider these scenarios:
- Persistent abdominal bloating or irregular bowel movements alongside borderline metabolic labs.
- Family history of autoimmune or inflammatory bowel disease with emerging metabolic risk factors.
- Patients already on lipid‑lowering meds who still have high triglycerides despite diet adherence.
Discuss these with a gastroenterologist; they’ll decide if a stool calprotectin or a blood zonulin test makes sense.
Lifestyle Factors That Modify the Indicators
Nutrition – the metabolic‑friendly plate
Picture a colorful plate: half leafy greens, a quarter lean protein, a quarter whole‑grain carbs, plus a drizzle of olive oil and a sprinkle of nuts. That simple visual can keep your blood sugar steady, raise HDL, and trim triglycerides. Bonus: fiber feeds the good gut bacteria we just talked about.
Physical activity – how much is enough?
The CDC recommends at least 150 minutes of moderate‑intensity aerobic exercise per week (think brisk walking, cycling, or dancing) plus two strength‑training sessions. Consistent movement improves insulin sensitivity, helps shrink waist circumference, and boosts HDL by up to 10 %.
Sleep & stress – hidden drivers
Less than 7 hours of sleep or chronic stress spikes cortisol, a hormone that encourages fat storage around the midsection. Try a wind‑down ritual: dim lights, no screens 30 minutes before bed, and a few minutes of deep breathing. Small changes can have a surprisingly big impact on those metabolic numbers.
Smoking & alcohol – impact on HDL & triglycerides
Smoking lowers HDL and damages blood vessels, while excess alcohol can shoot triglycerides sky‑high. Cutting back, or ideally quitting smoking, is a win‑win for your metabolic health.
Testing & Diagnosis – From Clinic to Home
Standard blood panel components you’ll see
A typical fasting panel includes:
- Glucose
- HbA1c (average glucose over 3 months)
- Lipid profile (HDL, LDL, triglycerides)
- C‑reactive protein (CRP) – a general inflammation marker
Physical exam measurements
During a routine check‑up, the provider will measure your waist with a flexible tape and record blood pressure with an appropriately sized cuff. If you want to keep tabs at home, invest in a reliable digital cuff and a soft tape measure; consistency is key.
When to use advanced GI‑tract tests
If you have “borderline” metabolic labs and ongoing digestive discomfort, ask about stool calprotectin or serum zonulin. These tests can uncover hidden inflammation that may be sabotaging your metabolic progress.
Interpreting results – a simple decision tree
1️⃣ Three or more classic indicators → Metabolic syndrome diagnosis.
2️⃣ Two indicators + abnormal GI biomarker → Consider early intervention, even if full syndrome not met.
3️⃣ One indicator + healthy lifestyle → Focus on targeted changes (e.g., diet, exercise).
4️⃣ No indicators → Keep up the good work and annual screening.
Putting It All Together – Your Action Plan
7‑Step “Metabolic‑Check” Routine
| Step | What to Do |
|---|---|
| 1️⃣ Measure waist | Use a tape; record inches. |
| 2️⃣ Check blood pressure | Take two readings, five minutes apart. |
| 3️⃣ Fasted blood glucose | Lab draw after an overnight fast. |
| 4️⃣ Lipid panel | Get HDL and triglycerides checked. |
| 5️⃣ Review diet | Log meals for three days; look for hidden sugars. |
| 6️⃣ Consider GI biomarkers | If digestive symptoms exist, ask about calprotectin or zonulin. |
| 7️⃣ Follow‑up | Schedule a review with your provider within 3‑6 months. |
How to talk to your healthcare provider
“I’ve been tracking my waist and blood pressure, and I’m concerned about metabolic syndrome. Can we review my labs together and discuss whether gut‑health testing might give us extra insight?” Using clear language helps your clinician understand your goals and tailor a plan.
Trusted resources & tools
Beyond the medical visits, many reputable apps let you log waist, blood pressure, and food intake. For deeper gut insight, explore inflammation biomarkers and the GI‑trackers linked there.
Conclusion
Metabolic syndrome indicators aren’t just numbers on a lab report—they’re clues that your body is sending you about hidden risks. By understanding the five classic signs, paying attention to emerging gut biomarkers, and making intentional lifestyle tweaks, you can rewrite the story before it turns into heart disease, diabetes, or stroke. Take the 7‑step Metabolic‑Check, talk openly with your doctor, and remember: small, consistent steps add up to big health wins. You’ve got this, and we’re cheering you on every step of the way.























Leave a Reply
You must be logged in to post a comment.